| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website http://www.jcgo.org |
Case Report
Volume 1, Number 1, February 2012, pages 28-29
Angiofibroma of Vagina During Pregnancy Presenting as Antepartum Haemorrhage: A Case Report
Vellanki Venkata Sujathaa, b, Satyanarayana Veeragandhama
aKamineni Institute of Medical Sciences, Sreepuram, Narketpally, Nalgonda; Andhra Pradesh-508254, India
bCorresponding author: Vellanki Venkata Sujatha, D1/08, Doctors Quarters, Kamineni Institute of Medical Sciences, Sreepuram, Narketpally, Nalgonda; Andhra Pradesh-508254, India
Manuscript accepted for publication September 7, 2011
Short title: Angiofibroma of Vagina
doi: https://doi.org/10.4021/jcgo2e
| Abstract | ▴Top |
Cellular angiofibroma of the vulva is a rare tumor that was first described in 1997. It occurs in middle-aged women (average age: 47 years), has small size (less than three centimeters) and well-circumscribed margins. We report a rare case of vaginal angiofibroma presenting as antepartum haemorrhage at 34 weeks of gestation in a 20 year south Indian pregnant women. The differential diagnoses for this tumor include aggressive angiomyxoma, angiomyofibroblastoma, lipoma of fusiform cells, solitary fibrous tumor, perineurioma and leiomyoma.
Keywords: Angiofibroma; Neoplasm; Vagina; Pregnancy
| Introduction | ▴Top |
Vaginal angiofibroma is a rare benign tumour of the reproductive age but should be considered as a rare differential diagnosis of antepartum haemorrhage when it gets infected or following coitus.
Angiomyofibroblastoma is a soft tissue tumour that occurs mainly, but not exclusively, in the vulval region of premenopausal women [1]. Cellular angiofibroma is a rare tumour described for the first time by Nucci et al. in 1997 [2]. It consists of a tumoural mass of small size that is generally well circumscribed, and it typically arises in middle-aged patients. The differential diagnoses for this neoplasia include aggressive angiomyxoma, angiomyofibroblastoma, lipoma of fusiform cells, fibrous tumors, perineurioma and leiomyoma. This differentiation is done by means of the histological and immunohistochemical characteristics. We report a case arising in the vagina during pregnancy to draw the attention of pathologists and obstetricians to the fact that this rare neoplasm can occur outside the vulva.
| Case Report | ▴Top |
A 20 year south Indian primigravida with 34 weeks of gestation reported to the emergency pregnancy assessment unit with complaints of pain in the lower abdomen and low back ache since one day duration. She gives history of mass per vagina since two months duration. She gives history of vaginal bleeding since two days. The bleeding was moderate in amount. There was no history of diarrhoea, fever, urinary complaints or any recent illness. She was married since nine months. Her menstrual cycles were regular. She conceived spontaneously. She had regular antenatal checkups. Her first and second trimesters were uneventful. No significant past medical and surgical history noted.
On examination, patient was conscious, coherent with pulse 108/min, blood pressure 110/80 mmHg, temperature normal, cardiovascular and respiratory systems normal. Abdominal examination revealed fundal height corresponding to 34 weeks gestation. Uterus was irritable and tense. There was a single fetus in longitudinal lie with vertex presentation. Fetal heart rate was good and regular. On vaginal examination, an oedematous tender growth of 5 × 4 cm was seen at the introitus which was not reducible. The mass was bleeding on touch. A differential diagnosis of cervical infected pedunculated myoma, vaginal growth, placental abruption and cervical prolapse were made.
Her blood investigations were normal except for a raised total leucocyte count of 16.5 × 109 /L. Urine examination showed 5 - 6 pus cells and subsequent culture revealed no growth. Non stress test was reactive.
Ultrasound scan showed a single live intrauterine foetus in cephalic presentation of 33 weeks gestation with estimated fetal weight of 2208 g. Placenta was anterior upper segment with grade II maturity with no evidence of retroplacental clot. Liqour was adequate. An isoechoic mass of 5 × 4 cm was seen arising from the lateral vaginal wall with increased vacularity on Doppler was seen. She was given two doses of steroid for fetal lung maturity. She was on complete bed rest with foot end elevation and vulval pad was kept soaked in saline. The vaginal mass reduced in size to 3 × 4 cm. Her pregnancy continued till term and she delivered an alive female baby of birth weight 2.7 kg by caesarean section. The vaginal mass was seen arising from the upper right vaginal wall of 3 × 4 cm. Complete excision of the growth was done and sent for histopathological examination. Histopathological examination showed angiofibroma of vagina (Fig. 1).
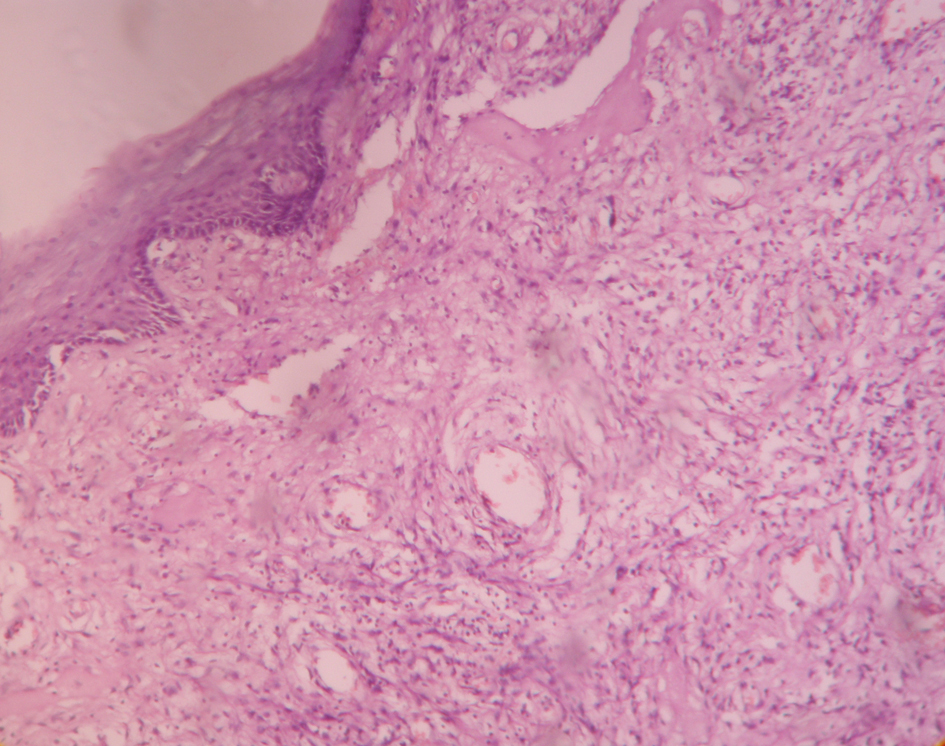 Click for large image | Figure 1. Showing vaginal epithelium with fibroblastic stroma and thin walled blood vessels. |
| Discussion | ▴Top |
Superficial vaginal angiomyofibroblastoma can be mistaken for an aggressive angiomyxoma, cellular angiofibroma and endometrial stromal sarcoma. Superficial myofibroblastoma of the lower female genital tract probably belongs to the morphological spectrum of vulvovaginal stromal polyps. Variegated patterns are described including myxoid, lace-like, sieve-like, fascicular, or storiform [3, 4]. The histomorphological features unique to this tumour are its superficial subepithelial location, good margination, and multipatterned growth of uniform, spindled and stellate shaped cells, varying sized blood vessels and highly collagenous and focally myxoid stroma. The immunohistochemical study showed positivity only for vimentin, which suggests, according to the literature, that the tumor cells are of fibroblastic origin.The lesion usually presents as a polypoidal or nodular mass in the cervix or the vagina usually in the fifth to eighth decade unlike in our case it presented in the early second decade [5].Our patient presented with a mass outside the vagina which was bleeding and haemorrrhagic and she had features of hyperdynamic circulation like tachycardia which made us think as a case of abruption placenta or an infected cervical polyp or prolapse which was not reducible. On further work up with ultrasound scan and Doppler we felt that it was a vaginal growth/polyp and then we aimed at continuation of pregnancy once the acute episode of bleeding stopped. With the histopathology we could arrive at a diagnosis of angiofibroma. The tumour has an extremely low risk of recurrence if completely excised [6]. We followed our case for two years before reporting.
Grant Support
None.
Conflicts of Interest
None.
| References | ▴Top |
- Micheletti AM, Silva AC, Nascimento AG, Da Silva CS, Murta EF, Adad SJ. Cellular angiofibroma of the vulva: case report with clinicopathological and immunohistochemistry study. Sao Paulo Med J. 2005;123(5):250-252.
pubmed doi - Nucci MR, Granter SR, Fletcher CD. Cellular angiofibroma: a benign neoplasm distinct from angiomyofibroblastoma and spindle cell lipoma. Am J Surg Pathol. 1997;21(6):636-644.
pubmed doi - Laskin WB, Fetsch JF, Tavassoli FA. Superficial cervicovaginal myofibroblastoma: fourteen cases of a distinctive mesenchymal tumor arising from the specialized subepithelial stroma of the lower female genital tract. Hum Pathol. 2001;32(7):715-725.
pubmed doi - Ganesan R, McCluggage WG, Hirschowitz L, Rollason TP. Superficial myofibroblastoma of the lower female genital tract: report of a series including tumours with a vulval location. Histopathology. 2005;46(2):137-143.
pubmed doi - McCluggage WG, White RG. Angiomyofibroblastoma of the vagina. J Clin Pathol. 2000;53(10):803.
pubmed doi - Chakravarty U S, Dhurde A V, Vartak SS, Badarkhe G, Veer S. Vaginal Angiomyofibroblastoma. Bombay Hospital Journal, Vol. 50, No. 1, 2008.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.