| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website http://www.jcgo.org |
Case Report
Volume 3, Number 4, December 2014, pages 143-146
Hyperemesis Gravidarum: An Out of the Box Presentation, a Rare Case Report and Literature Review
Sangeetha Thariana, g, Nayana Georgeb, Benjamin Tharianc, Kavitha Thariand, Benny Paule, Valsamma Chackof
aDepartment of Obstetrics and Gynaecology, Cochin Medical College, Ernakulam, Kerala, India
bDepartment of Medicine, Western Hospital, 148 Gordon Street, Footscray, Melbourne, Australia
cFlorida Hospital Centre for Interventional Endoscopy, Orlando, FL, USA
dDepartment of Pediatrics, Diana Princess of Wales Hospital, Grimsby, UK
eDepartment of CVTS, Amrita Institute of Medical Sciences, Ernakulam, Kerala, India
fDepartment of Obstetrics and Gynaecology, Kerala Institute of Medical Sciences, Trivandrum, Kerala, India
gCorresponding Author: Sangeetha Tharian, Department of Gynaecology, Cochin Medical College, HMT Colony P.O., Kalamassery, Ernakulam, Kerala 683 503, India
Manuscript accepted for publication October 17, 2014
Short title: Hyperemesis Gravidarum
doi: http://dx.doi.org/10.14740/jcgo287w
| Abstract | ▴Top |
Infratentorial ependymoma presenting as hyperemesis gravidarum during pregnancy is not reported in the literature. The management of these rare infratentorial tumors during pregnancy poses a great challenge to the obstetrician, since the physiological and hormonal changes of pregnancy can exacerbate the symptoms of the tumor and pose varying risks to both the mother and the fetus. We report a case of an infratentorial ependymoma presenting as hyperemesis gravidarum at 24 weeks of gestation. A 36-year-old diabetic woman was admitted with persistent vomiting at 24 weeks of gestation with a provisional diagnosis of hyperemesis gravidarum. She had history of hyperemesis gravidarum throughout the antenatal period and was on regular follow-up by obstetrician and physician. She developed features of intracranial hypertension and bilateral abducent nerve palsy during hospital stay. An MRI scan of the brain revealed a tumor of the fourth ventricle causing obstructive hydrocephalus. An emergency ventriculoperitoneal shunt was done to relieve the intracranial pressure. Subsequently, she underwent a suboccipital craniotomy with complete removal of the tumor. Histopathology was consistent with ependymoma. During the postoperative period, she developed stridor and dyspnoea and was ventilated. Intrauterine death of the fetus was confirmed by ultrasonology as there was cessation of the fetal heart sound. A hysterotomy was done to remove the fetus as an induction of labor failed. She subsequently developed ventilator associated pneumonia and adult respiratory distress syndrome followed by septicemia and expired on the 12th postoperative day despite appropriate antibiotics and other supportive measures. To our knowledge, this is the first reported case of infratentorial ependymoma presenting during pregnancy. Intracranial tumors, especially infratentorial tumors during pregnancy, are associated with high maternal and fetal morbidity and mortality as they behave differently from supratentorial tumors. A definite protocol for the management of pregnant patients with infratentorial tumors is lacking as there are only few reported cases. Early detection and treatment plays an important role in the management of these tumors.
Keywords: Infratentorial tumor; Ependymoma; Hyperemesis gravidarum; Intracranial hypertension
| Introduction | ▴Top |
Infratentorial ependymoma presenting as hyperemesis gravidarum during pregnancy is not reported in the literature. The management of these rare infratentorial tumors during pregnancy poses a great challenge to the obstetrician, since the physiological and hormonal changes of pregnancy can exacerbate the symptoms of the tumor and pose varying risks to both the mother and the fetus. We report a case of an infratentorial ependymoma presenting as hyperemesis gravidarum at 24 weeks of gestation.
| Case Report | ▴Top |
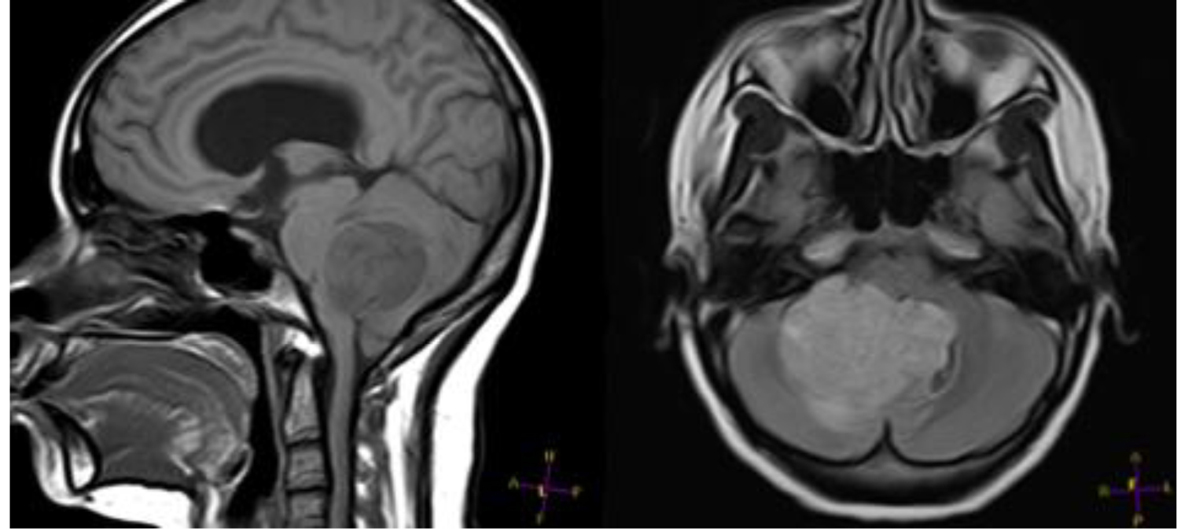
A 36-year-old woman with uncontrolled diabetes was admitted to our center at the 24th week of second pregnancy because of persistent vomiting and mild dehydration. She had history of hyperemesis gravidarum throughout the antenatal period which required three hospital admissions and was on regular follow-up by obstetrician and physician. There was no clinical or fundoscopic evidence of raised intracranial tension during her previous admissions in the antenatal period. She was admitted to the obstetrics department for symptomatic treatment. During the hospital stay, she developed disorientation. Intravenous thiamine was supplemented suspecting Wernicke’s encephalopathy as suggested by the physician. Subsequently she developed papilloedema and bilateral abducent nerve palsy without any focal neurological deficits. MRI scan of the brain revealed a tumor of the fourth ventricle causing obstructive hydrocephalus (Fig. 1).
She underwent an urgent ventriculoperitoneal shunt to relieve the intracranial pressure without any neurological complications. She improved symptomatically after the shunt. Subsequently she underwent an elective suboccipital craniotomy with complete removal of the tumor. The surgery was performed without any obstetric or neurologic complications. In the postoperative period, she had mild right hemiparesis. Histopathology examination was consistent with WHO grade II ependymoma (Fig. 2).
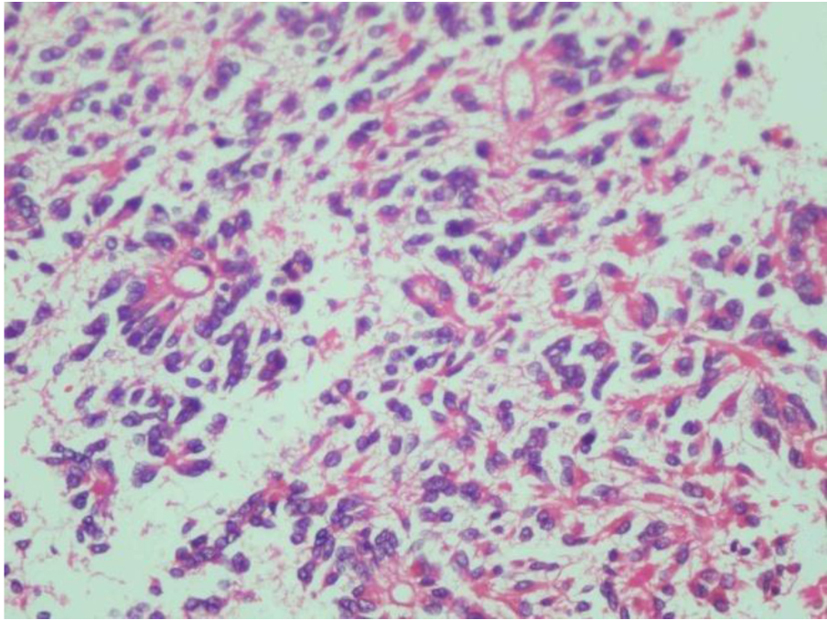 Figure 2. Typical perivascular pseudorosettes in ependymoma. Figure 2. Typical perivascular pseudorosettes in ependymoma. |
During the postoperative period, she developed leaking per vaginum and cessation of fetal heart sound. Ultrasound examination confirmed intrauterine fetal demise. A hysterotomy was done to remove the fetus as an induction of labor failed. A repeat MRI of brain revealed a hematoma at the floor of the fourth ventricle. Later she developed stridor for which she was electively ventilated. Subsequently she developed ventilator associated pneumonia and adult respiratory distress syndrome which was managed with appropriate antibiotics and mechanical ventilation. Unfortunately she developed septicemia and expired on the 12th postoperative day.
| Discussion | ▴Top |
Adult intracranial ependymomas are very rare and represent only 2-5% of all primary intracranial tumors [1]. Infratentorial ependymoma presenting as hyperemesis gravidarum during pregnancy is not reported in the English literature. The management of these rare infratentorial tumors during pregnancy poses a great challenge to the obstetrician. The physiological and hormonal changes of pregnancy can affect the size of the tumor which in turn can increase the intracranial pressure [2]. This can lead to rapid deterioration of the patient because of the location of the tumor in the posterior cranial fossa. They can be life-threatening as a result of the brainstem herniation due to raised intracranial pressure and can endanger the life of mother [2]. As ependymomas are very rare intracranial tumors, they have not been studied as comprehensively as other tumors.
The symptoms of infratentorial tumors like nausea and vomiting can mimic hyperemesis gravidarum [3]. Increased frequency of hyperemesis gravidarum in patients with brain tumors suggests that nausea and vomiting may be misattributed to the pregnancy itself in women with elevated intracranial pressure. But nausea and vomiting due to intracranial tumors usually appear later in pregnancy because of the mass effect of the intracranial tumor due to hemodynamic changes of pregnancy [4]. Another common presentation of pregnant women with brain tumors is seizure and hydrocephalus. This highlights the importance of a thorough examination for suspicious symptoms during pregnancy. Common sequelae of brain tumors like seizures, hydrocephalus, and aspiration pneumonia can have deleterious effects on pregnancy and they are more likely to have serious pregnancy complications like preterm labor, IUGR, and mortality. Pregnant patients with intracranial tumors usually experience more antenatal hospitalizations [5].
Our patient presented with symptoms at an earlier gestational age, and she suffered rapidly progressive neurological decline with signs of raised intracranial tension and involvement of the brainstem in the course of a few days. The latter was, to a large extent, due to the location of her tumor in the posterior fossa. Therefore, she required a more aggressive management, including a suboccipital craniotomy in the 24th week of gestation. Currently, there are no clear cut guidelines for the management of intracranial tumors in pregnant patients, especially posterior cranial fossa tumors, because the available evidence is limited to case reports or small patient series [6]. Therefore, decisionmaking in the management of these patients becomes extremely difficult and complex. Treatment of brain tumors during pregnancy depends on the site, type, and aggressiveness of the tumor and on balancing the complex and interconnected needs of mother and fetus [7]. A multidisciplinary team should recommend the optimal timing for the termination of pregnancy, as determined by the fetal maturity and mother’s neurological condition. Pregnant women with brain tumors are advised to delay radiotherapy and chemotherapy, which is the accepted treatment modality, until after delivery.
An algorithm to guide the management of pregnant patients with intracranial tumors was created in 2009 by Ng and Kitchen [8]. In the case of neurologically stable, first trimester pregnancies, the recommendation is to allow the pregnancy to continue until the second trimester or to terminate the pregnancy to facilitate radiotherapy and chemotherapy [8, 9]. In the first trimester surgical intervention is recommended only to relieve the raised intracranial pressure by a ventriculoperitoneal shunt or ventriculostomy. This helps to minimize the risk of anesthesia and surgery to the mother and fetus and allows the pregnancy to progress until the second trimester. In the second and early third trimester of pregnancy neurosurgical intervention for surgical removal of the mass is recommended if the tumor is large or there are signs of raised intracranial tension in stable patients [8, 9]. This is because of the lesser risk of intraoperative bleeding in the second trimester of pregnancy. As the maternal intravascular volume increases with advancing gestational age, tumor resection after second trimester can lead to significant bleeding. Furthermore, the risk of teratogenicity is less as the fetal organogenesis is completed by the end of first trimester. If the lesion is not large and the mother does not have intracranial hypertension or for benign tumors responding to corticosteroids, the tumor may be removed after delivery. However, if the patient is unstable or the prognosis is poor, immediate neurosurgical intervention is required regardless of the gestational age [8, 9]. Terry et al, in their retrospective study of an American obstetric population with intracranial tumors, determined that neurosurgical intervention during pregnancy helps the continuation of pregnancy to term [5]. Thus, there seems to be no compelling reason to delay indicated surgery because of concerns of adverse outcomes or risks to pregnancy.
Posterior fossa tumors like infratentorial ependymomas can lead to rapid deterioration because of the location and high risk of brain stem herniation. These patients may require early neurosurgical intervention compared to supratentorial tumors. Even minimal enlargement of the tumor due to physiological changes of pregnancy can lead to life-threatening complication like brain stem herniation. As majority of infratentorial tumors are entirely encapsulated and grow exophytically into the ventricle, complete removal of the tumor is possible in most of the cases [10]. Therefore, long-term survival after removal of infratentorial tumors is better compared to supratentorial tumors. Though posterior cranial fossa surgery can be performed in most patients with acceptable morbidity and mortality, surgical removal of the posterior fossa tumors carries a wider variety of complications when compared with tumors of the supratentorial compartment [11]. The overall postoperative mortality is approximately 2.6%. Most of the mortality is contributed by hematoma, edema with herniation, vascular compromise and resultant infarction or tumor progression. The remainder is attributed to aspiration pneumonia as a result of lower cranial nerve deficits and other medical conditions such as pulmonary embolism, myocardial infarction and sepsis [11]. As population-based studies are absent, it is not possible to quantify the risk of fetal loss, preterm labor, maternal mortality and other complications related to infratentorial tumors. Therefore pregnancies in patients with infratentorial tumors should be perceived as high risk and managed by an early scheduled caesarean delivery or labor induction. Management during delivery is also important as pushing can dramatically increase intracranial pressure and theoretically exacerbate cerebral edema or precipitate an intratumoral hemorrhage and brain stem herniation.
In conclusion, our case depicts the complexity of managing pregnant patients with infratentorial tumors. It clearly illustrates the diagnostic challenge and how the symptoms of raised intracranial tension may be mistaken for or might coexist with pregnancy related issues, such as hyperemesis gravidarum. Protean changes in the hormonal and physiological milieu inherent to the pregnant state can unmask these neoplasms. Therefore, it is very important to detect it and provide early care. Since there are no validated guidelines, it is extremely important for a multidisciplinary team of obstetricians and neurosurgeons to approach each case individually, in order to achieve the best results for the mother and the child. Obstetricians who care for pregnant patients with intracranial tumors, particularly infratentorial tumors, should be aware of the increased frequency of adverse pregnancy outcomes. Because of the challenges of studying a rare disease like infratentorial ependymoma, it is possible to predict the obstetric outcomes only by well-defined prospective studies.
Grant Support
No grants or financial support was accepted for this article.
Financial Disclosures
No financial assistance was accepted.
| References | ▴Top |
- Metellus P, Guyotat J, Chinot O, Durand A, Barrie M, Giorgi R, Jouvet A, et al. Adult intracranial WHO grade II ependymomas: long-term outcome and prognostic factor analysis in a series of 114 patients. Neuro Oncol. 2010;12(9):976-984.
doi pubmed - Johnson N, Sermer M, Lausman A, Maxwell C. Obstetric outcomes of women with intracranial neoplasms. Int J Gynaecol Obstet. 2009;105(1):56-59.
doi pubmed - Smith IF, Skelton V. An unusual intracranial tumour presenting in pregnancy. Int J Obstet Anesth. 2007;16(1):82-85.
doi pubmed - Stevenson CB, Thompson RC. The clinical management of intracranial neoplasms in pregnancy. Clin Obstet Gynecol. 2005;48(1):24-37.
doi - Terry AR, Barker FG, 2nd, Leffert L, Bateman BT, Souter I, Plotkin SR. Outcomes of hospitalization in pregnant women with CNS neoplasms: a population-based study. Neuro Oncol. 2012;14(6):768-776.
doi pubmed - Cohen-Gadol AA, Friedman JA, Friedman JD, Tubbs RS, Munis JR, Meyer FB. Neurosurgical management of intracranial lesions in the pregnant patient: a 36-year institutional experience and review of the literature. J Neurosurg. 2009;111(6):1150-1157.
doi pubmed - Esmaeilzadeh M, Dictus C, Kayvanpour E, Sedaghat-Hamedani F, Eichbaum M, Hofer S, Engelmann G, et al. One life ends, another begins: Management of a brain-dead pregnant mother-A systematic review. BMC Med. 2010;8:74.
doi pubmed - Ng J, Kitchen N. Neurosurgery and pregnancy. J Neurol Neurosurg Psychiatry. 2008;79(7):745-752.
doi pubmed - Elwatidy S, Jamjoom Z, Elgamal E, Abdelwahab A. Management strategies for acute brain lesions presenting during pregnancy: a case series. Br J Neurosurg. 2011;25(4):478-487.
doi pubmed - Fokes E, Earle K. Ependymomas - Clinical and pathologic aspects. J Neurosurgery. 1969;30:585-594.
doi pubmed - Dubey A, Sung WS, Shaya M, Patwardhan R, Willis B, Smith D, Nanda A. Complications of posterior cranial fossa surgery--an institutional experience of 500 patients. Surg Neurol. 2009;72(4):369-375.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.