| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website http://www.jcgo.org |
Case Report
Volume 5, Number 3, September 2016, pages 97-99
Bilateral Purtscher-Like Retinopathy With Profound Macular Ischemia and Vision Loss in Severe Pre-Eclampsia
Alexander Kotlyara, c, Sruthi Arepallib, Aleksandra V. Rachitskayab, Amanda Kalana
aDepartment of Obstetrics and Gynecology and Women’s Health Institute, Cleveland Clinic Foundation, Cleveland, OH 44195, USA
bCole Eye Institute, Cleveland Clinic Foundation, Cleveland, OH 44195, USA
cCorresponding Author: Alexander Kotlyar, Department of Obstetrics and Gynecology and Women’s Health Institute, Cleveland Clinic Foundation, Cleveland, OH 44195, USA
Manuscript accepted for publication August 25, 2016
Short title: Purtscher-Like Retinopathy in Pre-Eclampsia
doi: http://dx.doi.org/10.14740/jcgo410w
| Abstract | ▴Top |
Purtscher-like retinopathy is an extremely rare condition in patients with pre-eclampsia. The bilateral vision loss as seen in the current case is infrequent, but devastating. Our patient is a 27-year-old healthy primigravida patient with severe pre-eclampsia undergoing uncomplicated cesarean section due to abnormal kidney function and worsening hypertension. Postoperatively, she developed Purtscher-like retinopathy with profound macular ischemia and count-finger only vision. Neuroimaging was unrevealing. Her postoperative course was significant for hyponatremia, acute kidney injury, ileus, pancreatitis, leukocytosis, and postoperative fevers with suspected septic pelvic thrombophlebitis. The resultant visual acuity overall improved, but remained limited to 20/150 and 20/250 at 3 months postpartum. Purtscher-like retinopathy in the setting of pre-eclampsia can result in vision loss even in the absence of findings on neuroimaging or presence of HELLP syndrome.
Keywords: Purtscher-like retinopathy; Pre-eclampsia; Vision loss
| Introduction | ▴Top |
Visual changes in pregnant patients with pre-eclampsia and eclampsia could be of various etiologies. Most commonly, they are transient and are associated with serous retinal detachments, focal necrosis of retinal pigment epithelium, and cortical blindness. These tend to resolve with little visual sequelae. Vascular occlusive disease is a more rare occurrence [1]. Purtscher-like retinopathy has been reported in a few previous case reports [2-7]. In some of the reported cases, the visual acuity spontaneously improved albeit not to baseline. The current case is unique as the patient developed profound bilateral macular ischemia and visual loss due to Purtscher-like retinopathy in the setting of pre-eclampsia and in the absence of HELLP syndrome or any findings on neuroimaging.
| Case Report | ▴Top |
A 27-year-old primigravida patient with past medical history significant only for controlled asthma presented at 31 and 3/7 weeks with blood pressures (BPs) of 180 s/110 s. Pre-eclampsia labs were notable for a protein-to-creatinine ratio of 11.6 and a uric acid of 7.9 mg/dL. Her 24-h urine protein collection was notable for 7 g of protein with a creatinine clearance of only 67.9 mL/min and volume 750 mL. Serum creatinine upon presentation was 0.87 mg/dL. She was treated with hydralazine and started on labetalol to maintain BP control. Betamethasone for fetal lung maturity and magnesium for fetal neuroprotection was administered. Ultrasound showed intrauterine growth restriction with normal umbilical artery Doppler assessment and a biophysical profile (BPP) of 8/10, with two points off for lack of fetal breathing.
She remained overall stable aside from a mild increase in her serum creatinine from 0.86 to 1.04 mg/dL. On hospital day 5, she exhibited labile hypertension and onset of headache. This led to the decision to start labor induction with cervidil. Following 12 h of cervidil, minimal cervical change was seen with her Bishop score remaining at 3 (1.5 cm/60%/-2). A Cook bulb catheter was placed which successfully led to further cervical ripening. Throughout this time, the patient’s fetal heart tracing showed minimal variability which prompted the decision to perform low-transverse cesarean delivery. There were no intraoperative complications with one episode of mild hypotension down to the 90 s/60 s. The 1-min and 5-min Apgar scores were 7 and 8. She was restarted on her antepartum dose of labetalol and magnesium. On the evening of her cesarean section, her serum sodium decreased to 127 mmol/L for which she received normal saline.
On postoperative day 1, her urine output decreased. Her magnesium level was found to be greater than 9.6 mEq/dL, and the patient became increasingly somnolent. Magnesium was discontinued, subsequent ECG was unremarkable and chest X-ray did not show any pulmonary edema. On the evening of postoperative day 2, she remained somnolent and complained of an inability to see. In addition, she became hypertensive and was treated with low dose hydralazine for BPs 160 s/100 s. Given her emerging hyperkalemia to 5.6 mEq/dL, she was given sodium polystyrene and a second ECG showed a normal sinus rhythm. Her cardiac enzymes remained within normal limits. Her lab work revealed hyponatremia and acute kidney injury which was treated with aggressive fluid hydration. Brain MRI showed patent intracranial venous sinuses and punctate T2 prolongation at midbrain of unclear etiology with “questionable hypothalamic pathology”. Upon evaluation by neurology, no new neurological deficits were found and the MRI findings were interpreted as secondary to artifact. EEG and carotid ultrasound were unremarkable.
Throughout her hospital course, she continued to be hyponatremic with acute kidney injury (peak creatinine of 1.4 mg/dL on postoperative day 9) and worsening generalized anasarca. Over the subsequent 20 days, her hypotnatremia resolved; however, she developed an ileus likely secondary to a mild pancreatitis, which resolved with conservative measures. Her white blood cell count fluctuated in excess of 20,000 cells/μL with repeatedly negative blood and urine cultures. She was febrile up to 39.3 °C. Her ESR was 80 and CRP was 30.3. Septic thrombophlebitis was suspected and she was started on a heparin drip and ampicillin and sulbactam. On postoperative day 24, she was afebrile and was medically stable for discharge to an acute rehabilitation unit. Throughout her hospital stay, no evidence of HELLP, HUS, or DIC syndromes was seen.
The ophthalmology service examined the patient the day she reported decreased visual acuity. Her vision was limited to counting fingers and her intraocular pressure was normal. No afferent pupillary defect was noted. The exam was significant for diffuse retinal whitening, optic nerve palor and retinal hemorrhages (Fig. 1A). Fluorescein angiography showed significant macular non-perfusion (Fig. 1B). At 3-month follow-up, the visual acuity remained limited to 20/150 and 20/250. Additional negative workup included hypercoagulability workup, rheumatologic workup, and transesophageal echocardiogram with the bubble study.
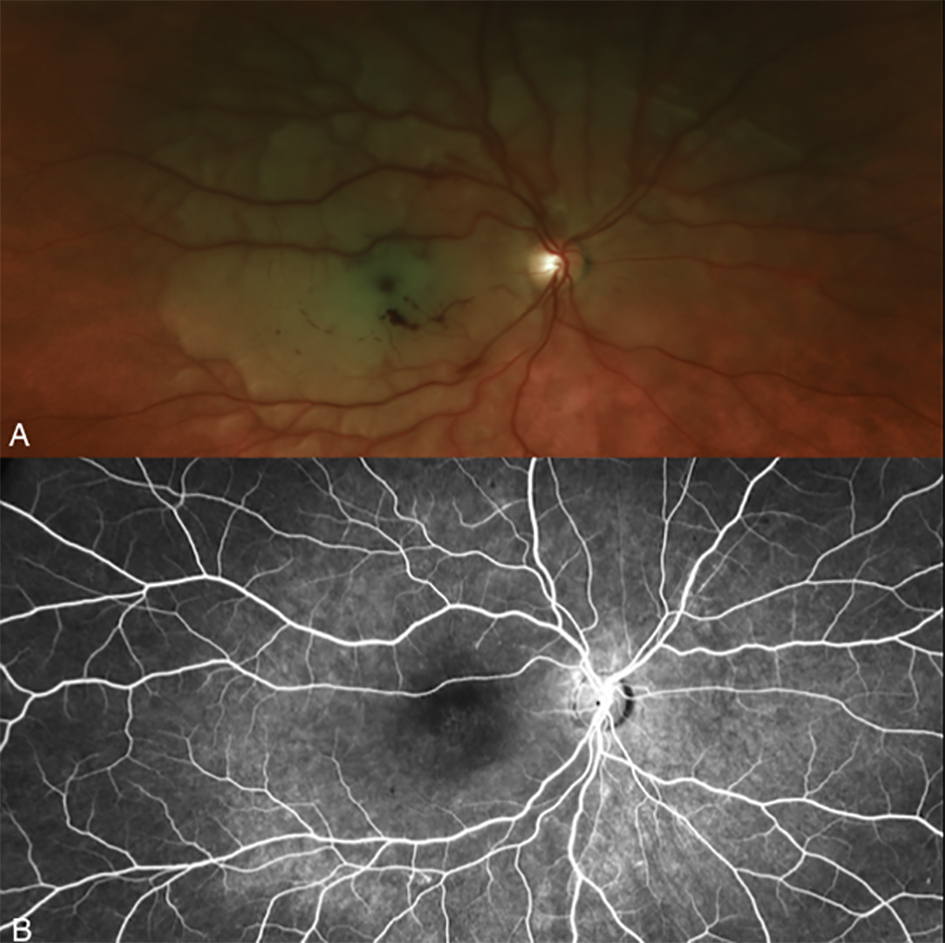 Click for large image | Figure 1. Fundus photo and fluorescein angiography (FA) of Purtscher-like retinopathy in pre-eclampsia. (A) Fundus photograph shows optic nerve pallor, diffuse retinal whitening and macular hemorrhages. (B) Mid-phase FA displays macular non-perfusion. |
| Discussion | ▴Top |
Some form of hypertension complicates 5-7% of all pregnancies [8]. Pre-eclampsia is characterized by hypertension and proteinuria. Eclampsia occurs in approximately 0.5% of women with mild preeclampsia and in approximately 2-3% of those with severe preeclampsia [8]. Visual symptoms have been described to occur in approximately 25% of pre-eclamptic and 19-45% of eclamptic women. The decrease in vision is usually transient [7]. Decreased vision is more commonly associated with serous retinal detachments, focal necrosis of retinal pigment epithelium, and cortical blindness. The etiology of the ocular manifestations is believed to be choroidal ischemia due to vasospasm. Arterial occlusive disease has also been reported even in patients without any risk factors [1]. An increase in the level of clotting factors and clotting activity occurs during pregnancy. While in retinal artery occlusion the larger retinal arteries are affected, in Purtscher-like retinopathy non-perfusion of smaller retinal arterioles or capillaries may be seen [1].
Purtscher-like retinopathy in the setting of pre-eclampsia was first described by Blodi et al [2]. Purtscher’s retinopathy is classically seen in trauma and is characterized by multiple areas of retinal whitening and intra-retinal hemorrhages [1]. In addition to pre-eclampsia, Purtscher-like retinopathy can be seen in acute pancreatitis, renal failure, fat embolism syndrome, and connective tissue disorders [1].
Since the report published by Blodi et al, there have been few additional reports on Purtscher-like retinopathy in pregnancy. It can occur in otherwise uncomplicated pregnancies barring pre-eclampsia and patients with severe eclampsia and seizures. Patients with HELLP syndrome and pancreatitis have been reported to develop Purtscher-like retinopathy [8]. It can also be associated with findings on neuroimaging consistent with brain infarcts [2-7]. The majority of patients are primigravidas, but some secundigravidas have been reported [4].
The exact pathophysiology of pre-eclampsia remains to be elucidated, but is considered to entail reduced organ perfusion and endothelial dysfunction [7]. Similarly, the exact cause of postpartum Purtscher-like retinopathy is unknown. It has been hypothesized that amniotic fluid exposure leads to C5a-activated leukoembolization [2].
The majority of cases focused on stabilization of the patients’ overall medical condition. Spontaneous visual improvement has been reported even from only being able to see only hand motion to 20/60. In one report where systemic steroids were used, no improvement in vision was noted [4]. One case of intravitreal steroid administration showed improvement, but authors commented that this could be due to spontaneous recovery [8]. In cases of Purtscher’s retinopathy from other causes, there also little evidence for systemic high dose steroids [1]. Most likely the visual prognosis depends on the degree of the original ischemia and perfusion of the macula [4].
Putting these prior reports into the context of our patient’s clinical course, we see how our patient exhibited an unusual variation in the presentation of bilateral vision loss in the setting of pre-eclampsia. Our patient presented with pre-eclampsia, underwent uncomplicated cesarean section, and on the second day after her surgery developed profound vision loss due to severe macular ischemia. The subsequent findings were consistent with Purtscher-like retinopathy. However, no significant findings were seen on neuroimaging which is in contrast to several prior reports of this form of retinopathy [2-7]. Her postoperative course was also notable for hyponatremia, acute kidney injury, ileus, pancreatitis, leukocytosis, postoperative fevers with suspected septic pelvic thrombophlebitis and postpartum depression. This complex series of medical complications is unusual among prior reports and lends further support that a systemic derangement, possibly as a consequence of pre-eclampsia can lead to sudden and profound visual loss. In contrast to a more recent report by Larra-Torres et al, our patient has shown some degree of visual improvement [5]. Otherwise her extensive workup was negative. Her vision improved to 20/150 and 20/250 at 3 months.
Purtscher-like retinopathy in the setting of pre-eclampsia is a rare visually devastating condition. Given the rarity of these cases, no preventive modalities are currently known. This case showcases several points. First, the majority of visual changes in pregnant patients with pre-eclampsia and eclampsia are transient. Second, Purtscher-like retinopathy in pregnancy is a rare condition that sometimes can be associated with visual recovery, but can also result in profound vision loss.
Acknowledgments
We would like to thank our colleagues from the Department of Obstetrics and Gynecology at the Cleveland Clinic who provided critical assessment of the manuscript and assisted in the literature search.
Abbreviations
ESR: Erythrocyte Sedimentation Rate; CRP: C Reactive Protein; HELLP: Hemolysis, Elevated Liver enzymes, and Low Platelets counts; HUS: Hemolytic Uremic Syndrome; DIC: Disseminated Intravascular Coagulation; ECG: Electrocardiogram; MRI: Magnetic Resonance Imaging
| References | ▴Top |
- Ryan Stephen, et al. Retina. 5th Edition. Philadelphia: Saunders; 2013.
- Blodi BA, Johnson MW, Gass JD, Fine SL, Joffe LM. Purtscher's-like retinopathy after childbirth. Ophthalmology. 1990;97(12):1654-1659.
doi - Moseman CP, Shelton S. Permanent blindness as a complication of pregnancy induced hypertension. Obstet Gynecol. 2002;100(5 Pt 1):943-945.
doi - Shaikh S, Ruby AJ, Piotrowski M. Preeclampsia-related chorioretinopathy with Purtscher's-like findings and macular ischemia. Retina. 2003;23(2):247-250.
doi pubmed - Lara-Torre E, Lee MS, Wolf MA, Shah DM. Bilateral retinal occlusion progressing to long-lasting blindness in severe preeclampsia. Obstet Gynecol. 2002;100(5 Pt 1):940-942.
doi pubmed - Landes A, Walter MJ. Purtscher-like retinopathy in a patient with preeclampsia. Seminars in Ophthalmology. Vol. 24. No. 4-5. London, UK: Informa UK Ltd; 2009.
- Shukla D, Maheshwari R, Ramchandani B, Kanungo S. Purtscher-like retinopathy with serous retinal detachment in preeclampsia of pregnancy: complications and management. Retin Cases Brief Rep. 2010;4(4):332-335.
doi pubmed - Jeon SY, Jung E, Seol HJ, Hur YJ. Development of Purtscher-like retinopathy after pre-eclampsia combined with acute pancreatitis. Obstet Gynecol Sci. 2013;56(4):261-264.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.