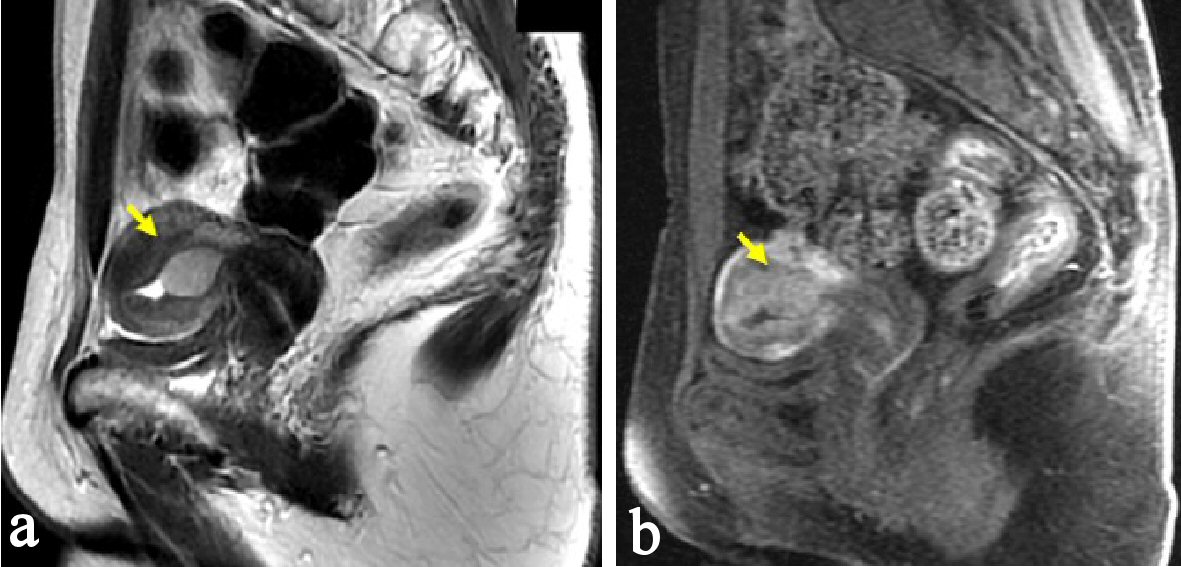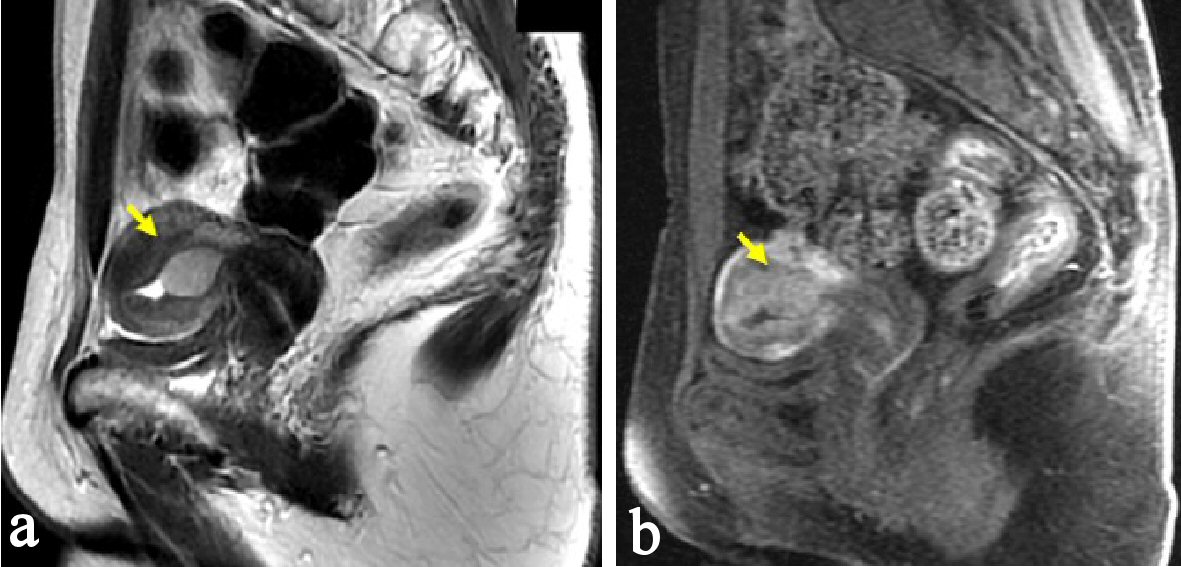
Figure 1. Pelvic MRI, sagittal section at the first consultation. (a) There is a low signal endometrial mass of 19 mm in diameter on T2-weighted sagittal section (arrow). (b) The endometrial mass was enhanced in contrast study (arrow). Myometrial invasion or uterine cervical invasion of the mass was not proven in MRI.
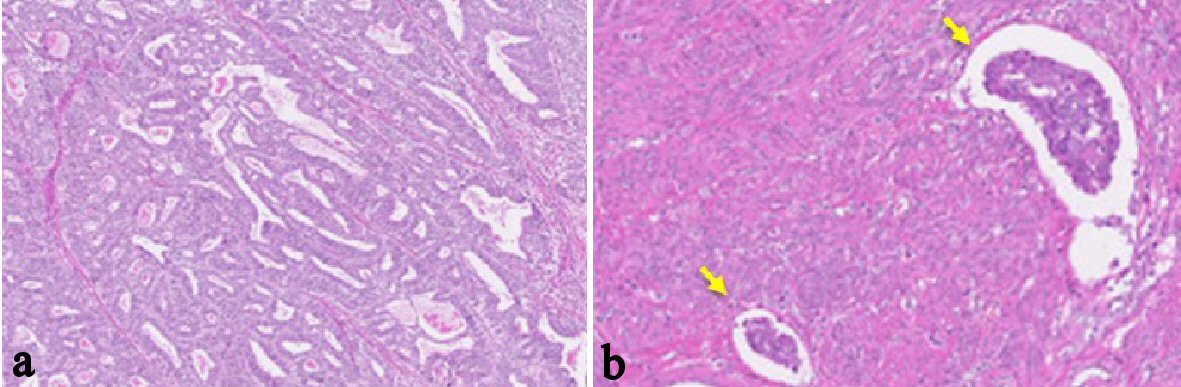
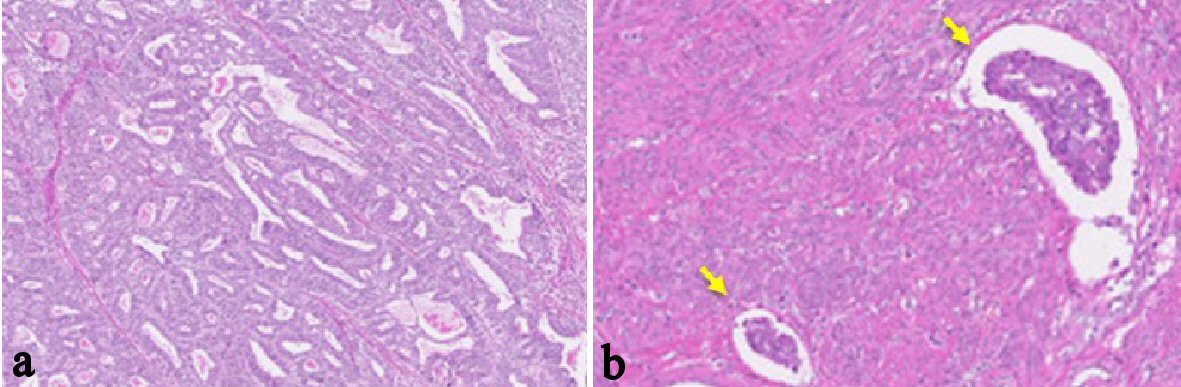
Figure 2. Histological findings of the endometrial tumor of surgically resected uterus (H&E stain; the original magnification is × 40). (a-b) Atypical glands are proliferating with tubular and cribriform pattern. There is no finding of papillary proliferation. The tumor had invaded into the myometrium within half of the muscular layer. There were findings of vascular space invasion and lymphatic vascular space invasion (b), (arrows). Postoperative diagnosis was endometrial adenocarcinoma grade 1, pT1aN0M0.
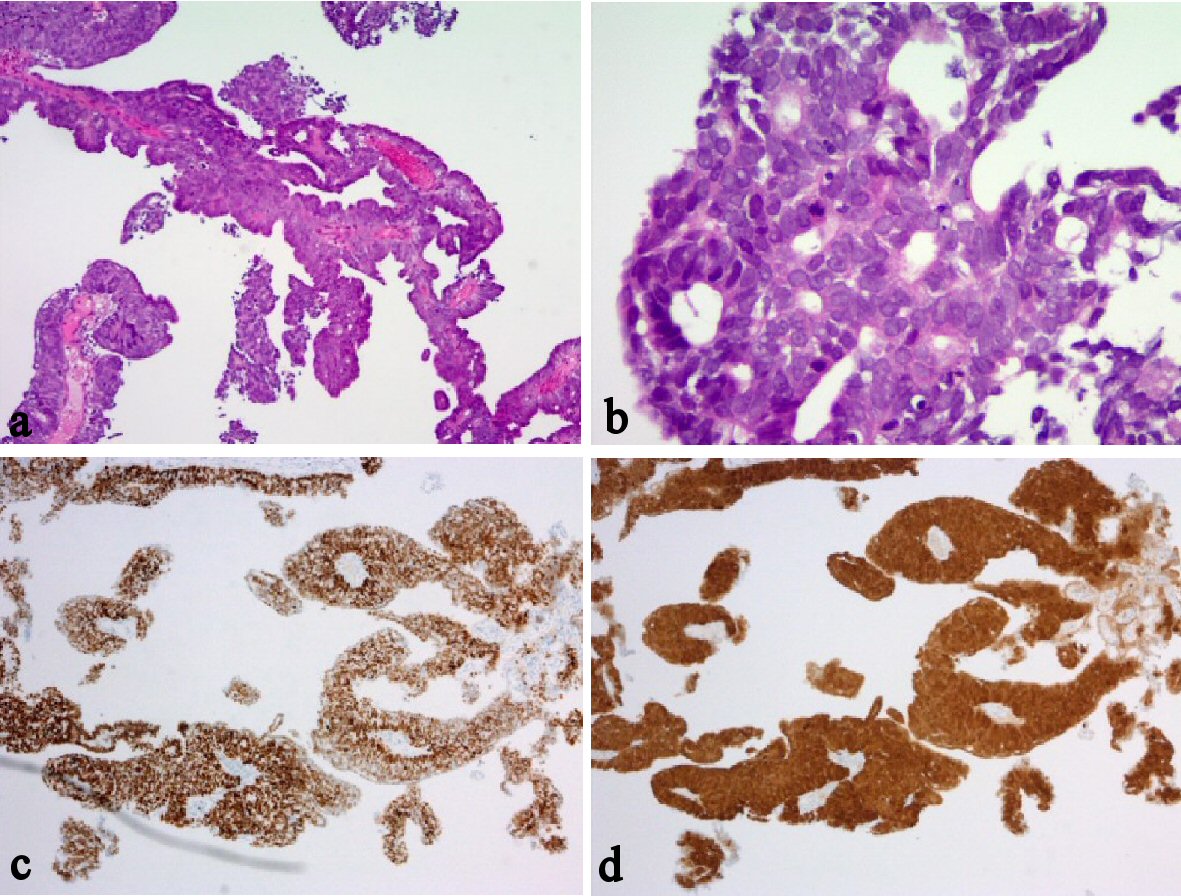
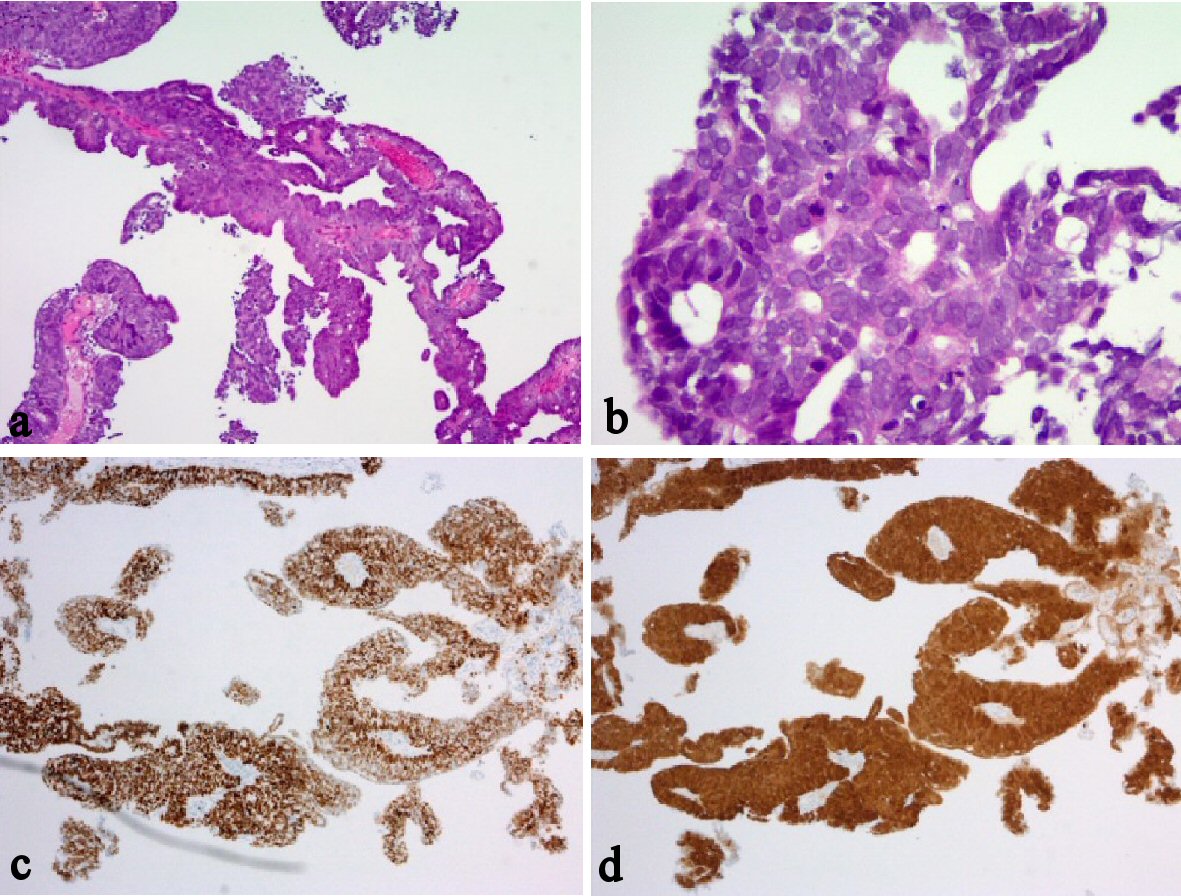
Figure 3. Histological and immunohistochemical findings of vaginal tumor. (a-b) H&E stain. (c) P53 immunohistochemistry. (d) P16 immunohistochemistry. The atypical cancer cells were proliferating with papillary appearance, with forming multiple layers (a-b); the original magnifications are × 40 and × 100, respectively. Immunostaining results of the vaginal tumor were positive for p53 (c), the original magnification is × 40; strongly positive for p16 (d), the original magnification is × 40; and negative for ER. Additionally, exactly same immunostaining results were obtained from the primary endometrial cancer, which was diagnosed as endometrioid adenocarcinoma (Figures not shown).