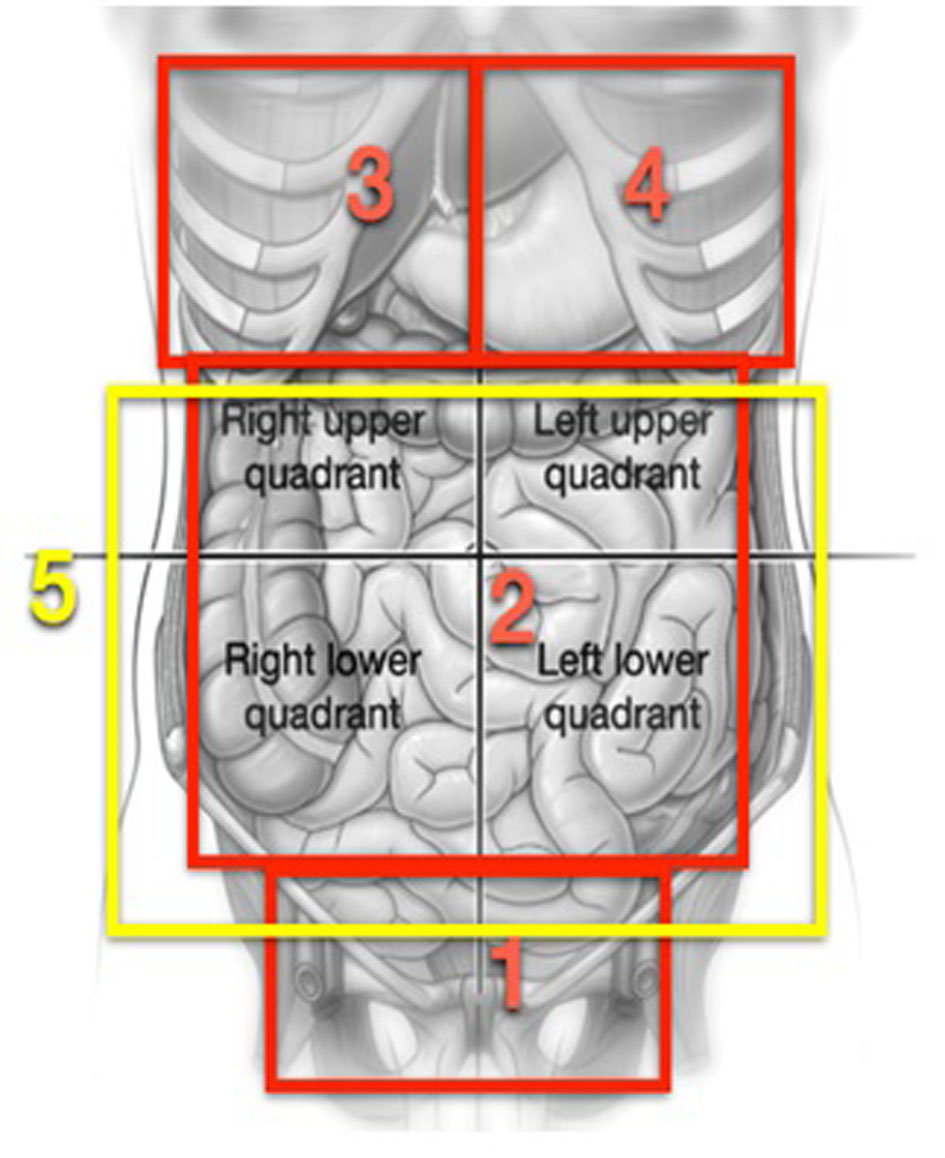
Figure 1. Graphs reproducing areas described in the process proposed by Morrow [8].
| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website http://www.jcgo.org |
Original Article
Volume 4, Number 3, September 2015, pages 251-257
Effectiveness and Safety of Cytoreduction Surgery in Advanced Ovarian Cancer: Initial Experience at a University General Hospital
Figures
Tables
| n = 34 | |
|---|---|
| Quantitative variables: median (range). Nominal variables: count (%). | |
| Age | 60 (41 - 84) |
| Tumor | |
| Primary | 22 (65%) |
| Recurrence | 12 (35%) |
| Serous/Papillary-Serous | 14 (41%) |
| Endometrioid | 5 (15%) |
| Granular | 1 (3%) |
| Mullerian | 1 (3%) |
| Neuroendocrine | 1 (3%) |
| Mixed | 1 (3%) |
| Peritoneal | 9 (26%) |
| Indistinct | 2 (6%) |
| FIGO | |
| IIIC | 18 (53%) |
| IV | 16 (47%) |
| ASA | |
| I | 1 (3%) |
| II | 9 (26%) |
| III | 23 (68%) |
| IV | 1 (3%) |
| IPC operative | 12 (2 - 33) |
| 1 - 10 | 13 (38%) |
| 11 - 20 | 13 (38%) |
| 20 | 8 (24%) |
| Primary | 14 (4 - 33) |
| Recurrence | 5 (2 - 24) |
| CEA | 2 (1 - 150) |
| CA199 | 17 (3 - 67) |
| CA125 | 254 (24 - 14,125) |
| CA153 | 115 (5 - 1,500) |
| Ascites (clinically evident) | 9 (26%) |
| Pleural spillage (radiological) | 7 (21%) |
| Intestinal subocclusion | 4 (12%) |
| Primary | 2 (9%) |
| Recurrence | 2 (17%) |
| Preoperative laparoscopy | 19 (56%) |
| IPC 1 - 10 | 6 (18%) |
| IPC 11 - 20 | 11 (32%) |
| IPC +20 | 2 (6%) |
| IPC 1 - 10 accuracy | 33% |
| IPC +10 accuracy | 63% |
| n = 34 | |
|---|---|
| Quantitative variables: median (range). Nominal variables: count (%). | |
| Visceral resections | 30 (88%) |
| Visceral resections per patient | |
| 0 | 5 (15%) |
| 1 | 1 (3%) |
| 2 | 9 (26%) |
| 3 | 5 (15%) |
| 4 | 3 (9%) |
| 5 | 2 (6%) |
| 7 | 5 (15%) visceral resections |
| 8 | 2 (6%) |
| 11 | 1 (3%) |
| 14 | 1 (3%) |
| Peritonectomy (all) | |
| Complete | 21 (62%) |
| Partial | 7 (21%) |
| No | 6 (17%) |
| Primary | |
| Complete | 18 (82%) |
| Partial | 3 (14%) |
| No | 1 (4%) |
| Relapse | |
| Complete | 3 (25%) |
| Partial | 4 (33%) |
| No | 5 (42%) |
| Duration of surgery (min) | 540 (280 - 750) |
| Primary | 540 (390 - 750) |
| Relapse | 480 (280 - 720) |
| Regulated lymphadenectomies | 27 (80%) |
| Lymph nodes analyzed | 26 (1 - 88) |
| Lymph nodes positive | 2 (0 - 36) |
| Infrarenal aorta caval lymphadenectomy | 27 (80%) |
| Lymph nodes analyzed | 12 (1 - 28) |
| Lymph nodes positive | 1 (0 - 12) |
| Left iliac pelvic lymphadenectomy | 23 (66%) |
| Lymph nodes analyzed | 7 (1 - 29) |
| Lymph nodes positive | 1 (0 - 11) |
| Right iliac pelvic lymphadenectomy | 22 (65%) |
| Lymph nodes analyzed | 7 (1 - 19) |
| Lymph nodes positive | 1 (0 - 15) |
| Supsramesocolic lymphadenectomy | 5 (15%) |
| Lymph nodes analyzed | 2 (1 - 9) |
| Lymph nodes positive | 1 (0 - 2) |
| Cytoreduction | |
| CC0 | 27 (79%) |
| CC1 | 4 (12%) |
| CC2 | 2 (6%) |
| CC3 | 1 (3%) |
| Cytoreducion CC0 | |
| Primary | 19 (70%) |
| Relapse | 8 (30%) |
| Cytoreduction CC1 | |
| Primary | 2 (50%) |
| Relapse | 2 (50%) |
| Cytoreduction CC2 | |
| Primary | 2 (100%) |
| Relapse | 0 |
| Cytoreduction CC3 | |
| Primary | 0 |
| Relapse | 1 (100%) |
| Complications | 19 (56%) |
| Digestive fistulas | 3 (9%) |
| Reoperation | 6 (18%) |
| Death 90 days | 2 (6%) |
| Stay in ICU | 6 (2 - 36) |
| Postoperative stay | 22 (8 - 63) |
| Stay > 20 days | 20 (59%) |
| Primary | 27 (10 - 56) |
| Relapse | 14 (8 - 63) |
| Organ | n | % |
|---|---|---|
| Sigmoid colon | 18 | 53 |
| Small intestine | 14 | 41 |
| Cecum and appendiz | 13 | 38 |
| Gallbladder | 12 | 35 |
| Rectum | 11 | 32 |
| Spleen | 11 | 32 |
| Transverse colon | 7 | 21 |
| Ascending colon | 5 | 15 |
| Pancreas body-tail | 5 | 15 |
| Hepatic peritoneum | 5 | 15 |
| Partial bladder | 4 | 12 |
| Descending colon | 4 | 12 |
| Liver | 4 | 12 |
| Diaphragm | 4 | 12 |
| Total bladder | 3 | 9 |
| Ureter | 3 | 9 |
| Major vessels | 3 | 9 |
| Stomach | 2 | 6 |
| Kidney | 2 | 6 |
| Adrenal | 2 | 6 |
| Total | 30 cases | 88% |