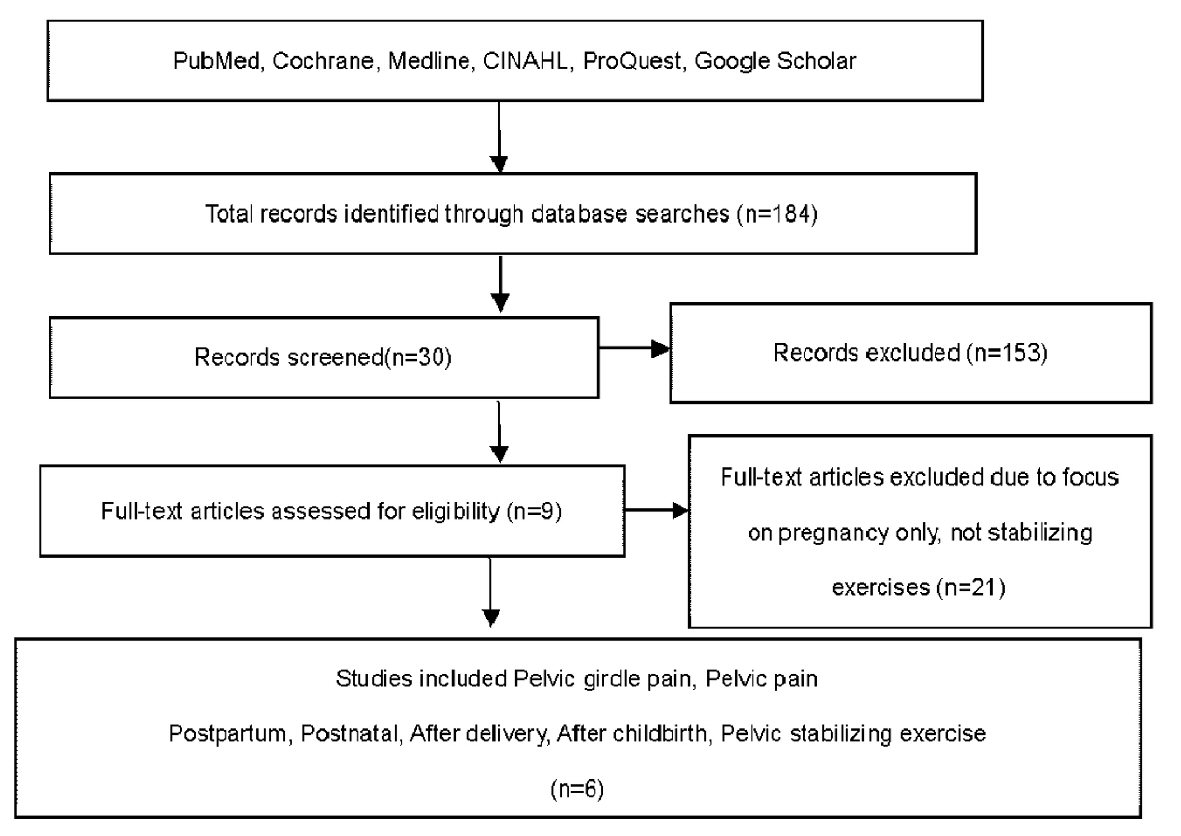
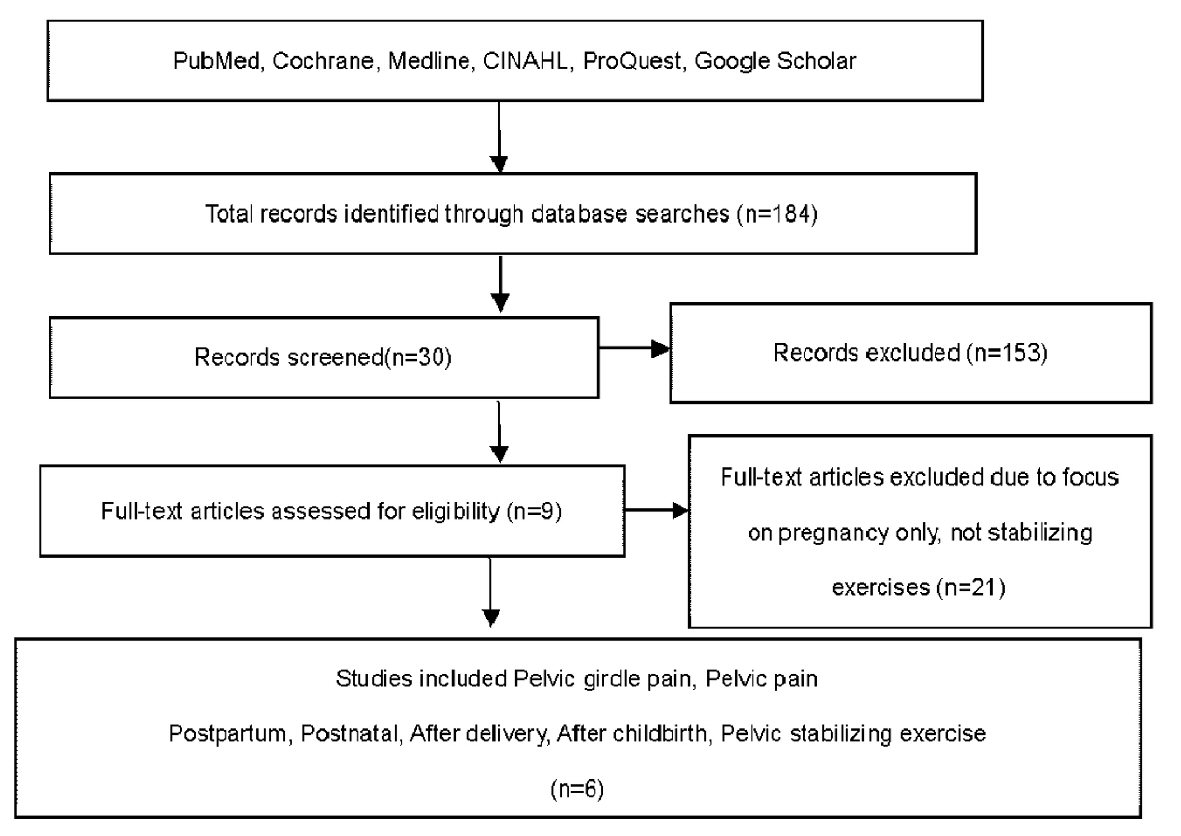
Figure 1. Literature search flow diagram.
| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website http://www.jcgo.org |
Review
Volume 8, Number 2, June 2019, pages 33-38
Are Pelvic Stabilizing Exercises Effective for Postpartum Pelvic Girdle Pain? A Literature Review
Figure
Table
| Study | Design | Subjects | Intervention | Results |
|---|---|---|---|---|
| Mens, JMA et al [11], 2000 | RCT | N = 44 women with PGP after pregnancy, 4.1 months after delivery | Group 1: performed exercises to increase the force of diagonal trunk muscle systems. | No differences between the three groups. 28 of 44 (63.6%) subjects improved; 12 (27.3%) were unchanged; 4 (9.1%) felt worse (P = 0.000). Decrease in pain scores from 36.3 to 28.6 (VAS) (P = 0.01), decrease in fatigue scores from 77.0 to 66.7 (P = 0.01). Physical mobility scale from 36.2 to 30.3 (P < 0.05). |
| Group 2: training of longitudinal trunk muscle systems without individual caching or pelvic belt; 30 min video tape. | ||||
| Group 3: No exercise. | ||||
| Frequency: 30 min video tape, 5 min interval, 3 times/day, 3 times/week, 8 weeks | ||||
| Duration: 8 weeks | ||||
| Stuge, B. et al [4], 2004 | RCT | N = 81 women with PGP 6 to 16 weeks after most recent delivery | Physical therapy focusing on specific stabilizing exercises (SSE) (joint mobilization, stretching, massage, relaxation, stretching, training TrA with coactivation of lumbar multifidus, latissimus dorsi, oblique abdominal muscles, erector spinae, quadratus, hip adductors, abductors. | After intervention and at 1 year postpartum, the SSE group showed improvement of pain and disability level and quality of life. |
| Frequency: 30 - 60 min, 3 days/week for 18 to 20 weeks | ||||
| Duration: 20 weeks | ||||
| Stuge, B. et al [12], 2004 | RCT | N = 81 women with PGP 6 to 16 weeks after most recent delivery | Physical therapy focusing on specific stabilizing exercises (joint mobilization, stretching, massage, relaxation, stretching, training TrA with coactivation of lumbar multifidus, latissimus dorsi, oblique abdominal muscles, erector spinae, quadratus, hip adductors, abductors. | |
| Frequency: 30 to 60 min, 3 days/week for 18 to 20 weeks | ||||
| Duration: 2 years | ||||
| Gutke, A. et al [13], 2010 | RCT | N = 88 women with PGP 3 months after delivery | Home exercises with specific stabilizing exercises (SSE group) (TrA, lumbar multifidus, PFM) local principles of motor learning theory 3 stages (target 3rd stage) | No significant differences at 3 - 6 months follow-up in either group. Pain frequency was improved at the 3-month follow-up (P = 0.011) mean hip extension and global muscle improved at the 3-month follow-up (P = 0.047) only in the SSE group. |
| Individual guidance by a physical therapist every second week | ||||
| Frequency: ≥ 2 times /day, each exercise 10 repetitions | ||||
| Duration: intervention period 3 months, outcome measured at 3 months after delivery, and 3, 6, 12, 24 months thereafter | ||||
| Control: individual exercise program | ||||
| Unsgaard-Tondel, M. et al [14], 2016 | RCT | N = 16 women with lumbopelvic pain 3 months after delivery | Tailored exercise therapy, including ultrasound-guided activation of deep muscles, strengthening and stretching exercises and advice. | Reduced pain and decreased disability over the intervention period. There was significant correlation between pain and disability (r = 0.89, P = 0.001), no correlation was observed between TrA activation and symptoms. |
| Frequency: 1 h and about 90 min/session, once a week | ||||
| Duration: 16 weeks | ||||
| Sakamoto et al [15], 2018 | RCT | N = 75 women 1 day after delivery | Exercises with a pelvic realignment device (Group R, n = 25), stabilization exercise (Group E, n = 25) a control group (Group C, n = 25) Frequency; 10 min/session, twice /day | Visual analogue scale score in Group R decreased significantly (P = 0.043). There were no significant differences between groups R and E (P = 0.66). The immediate and short-term effects of exercise in Group R showed greater improvements compared with those in Group E. |
| Duration: 4 weeks after delivery. |