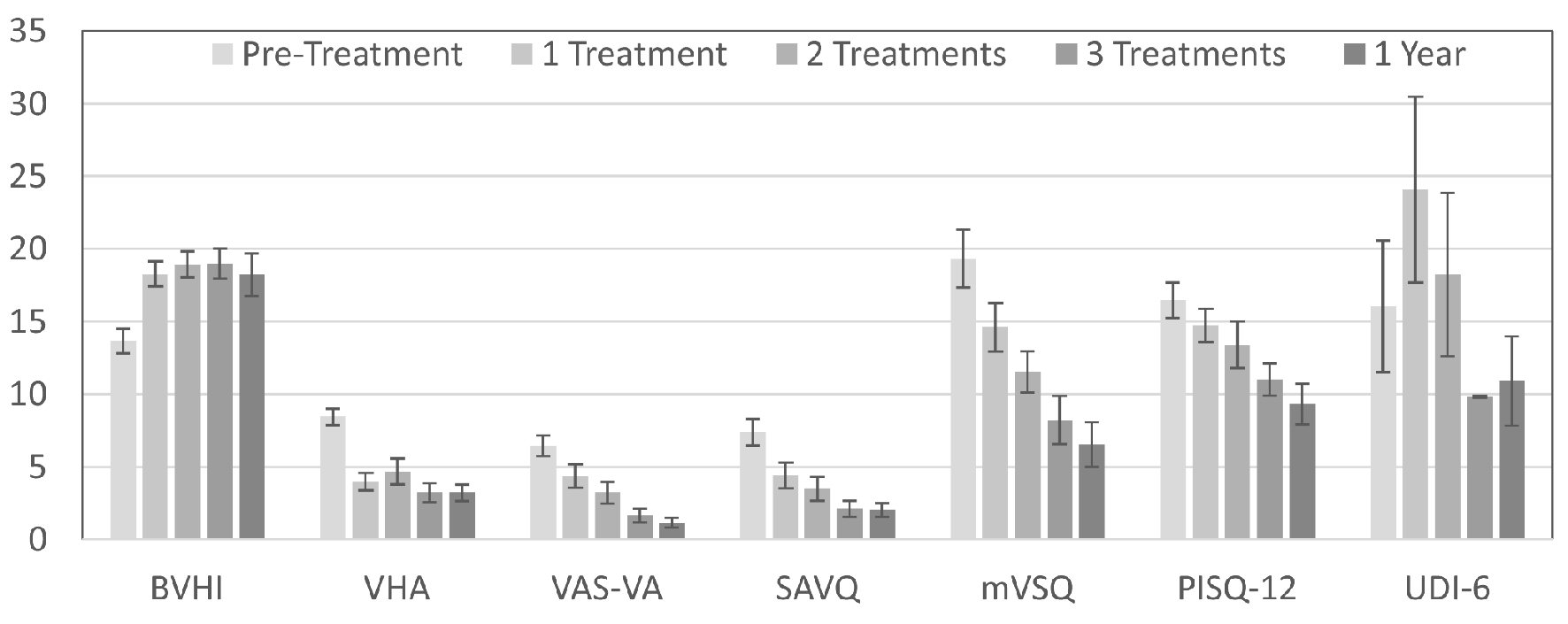
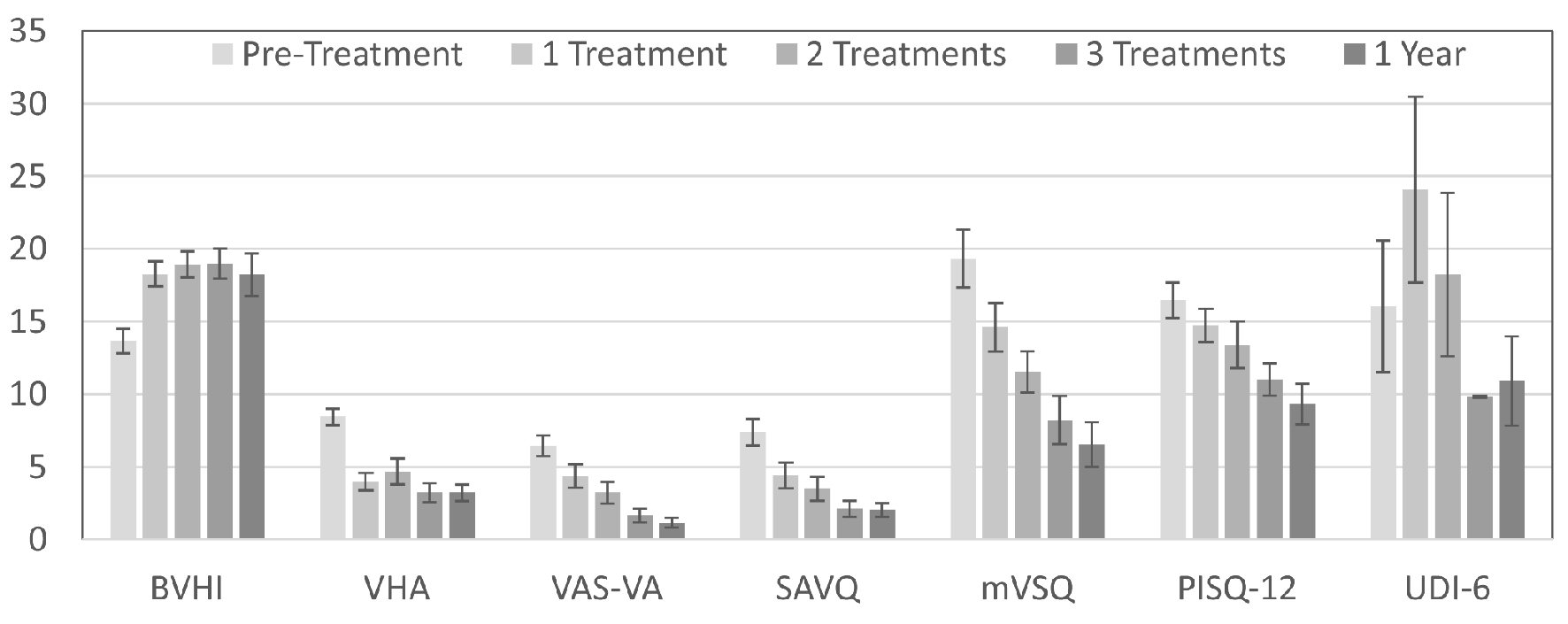
Figure 1. Change in GSM assessment scores over time with pixelated CO2 laser treatment. Lower scores indicate fewer or less severe symptoms for all assessments, except the BVHI.
| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website https://www.jcgo.org |
Original Article
Volume 10, Number 1, March 2021, pages 11-17
Prospective Study of Fractional Carbon Dioxide Laser Therapy for Symptoms of Genitourinary Syndrome of Menopause: One-Year Follow-Up
Figures
Tables
| Values presented are medians (25th, 75th percentiles), means ± standard deviation, or number (percent) of subjects, as appropriate. GSM: genitourinary syndrome of menopause. | |
| Age (years) | 58.3 ± 8.75 |
| Parity | 1 (1, 2) |
| Body mass index (kg/m2) | 25.5 ± 3.39 |
| Complained of stress urinary incontinence | 1 (6.7) |
| Complained of urge urinary incontinence | 3 (20.0) |
| History of breast cancer | 6 (40.0) |
| Previous hysterectomy | 5 (33.3) |
| Previously tried vaginal estrogen | 5 (33.3) |
| Smoking status | |
| Never | 12 (80.0) |
| Former | 3 (20.0) |
| Current | 0 (0.0) |
| Pelvic organ prolapse | |
| Stage 0 | 10 (66.7) |
| Stage 1 | 5 (33.3) |
| Assessment | Mean difference | 95% Confidence interval | P value |
|---|---|---|---|
| GSM: genitourinary syndrome of menopause; BVHI: Bachmann Vaginal Health Index; VHA: Vaginal Health Assessment; VAS-VA: visual analog grading scale for vaginal atrophy symptoms; SAVQ: Symptoms of Atrophic Vaginitis Questionnaire; mVSQ: modified Vulvovaginal Symptom Questionnaire; PISQ-12: Pelvic Organ Prolapse/Urinary Incontinence Sexual Function Questionnaire; UDI-6: Urinary Distress Inventory. | |||
| BVHI | 4.96 | 2.32, 7.60 | 0.002 |
| VHA | -5.00 | -6.78, -3.22 | 0.001 |
| VAS-VA | -4.85 | -6.61, -3.09 | 0.001 |
| SAVQ | -5.48 | -3.62, -7.34 | 0.001 |
| mVSQ | -12.44 | -16.33, -8.54 | < 0.001 |
| PISQ-12 | -5.45 | -8.16, -2.74 | 0.003 |
| UDI-6 | -7.64 | -16.3, 1.02 | 0.070 |
| Assessment | Mean difference | 95% Confidence interval | P value |
|---|---|---|---|
| GSM: genitourinary syndrome of menopause; BVHI: Bachmann Vaginal Health Index; VHA: Vaginal Health Assessment; VAS-VA: visual analog grading scale for vaginal atrophy symptoms; SAVQ: Symptoms of Atrophic Vaginitis Questionnaire; mVSQ: modified Vulvovaginal Symptom Questionnaire; PISQ-12: Pelvic Organ Prolapse/Urinary Incontinence Sexual Function Questionnaire; UDI-6: Urinary Distress Inventory. | |||
| BVHI | 4.55 | 0.66, 8.45 | 0.012 |
| VHA | -5.21 | -6.46, -3.97 | < 0.001 |
| VAS-VA | -5.46 | -7.11, -3.81 | 0.001 |
| SAVQ | -5.37 | -7.62, -3.12 | 0.001 |
| mVSQ | -12.80 | -16.98, -8.62 | < 0.001 |
| PISQ-12 | -7.11 | -10.80, -3.42 | 0.002 |
| UDI-6 | -5.13 | -14.83, 4.58 | 0.406 |
| Assessment | Mean difference | 95% Confidence interval | P value |
|---|---|---|---|
| GSM: genitourinary syndrome of menopause; BVHI: Bachmann Vaginal Health Index; VHA: Vaginal Health Assessment; VAS-VA: visual analog grading scale for vaginal atrophy symptoms; SAVQ: Symptoms of Atrophic Vaginitis Questionnaire; mVSQ: modified Vulvovaginal Symptom Questionnaire; PISQ-12: Pelvic Organ Prolapse/Urinary Incontinence Sexual Function Questionnaire; UDI-6: Urinary Distress Inventory. | |||
| BVHI | 0.88 | -1.80, 3.55 | 0.459 |
| VHA | 0.29 | -1.60, 2.17 | 0.660 |
| VAS-VA | -0.57 | -1.38, 0.24 | 0.219 |
| SAVQ | 0.00 | -0.89, 0.89 | 1.000 |
| mVSQ | -1.21 | -4.80, 2.38 | 0.336 |
| PISQ-12 | -0.49 | -2.80, 1.83 | 0.914 |
| UDI-6 | 3.27 | -2.56, 9.10 | 0.121 |