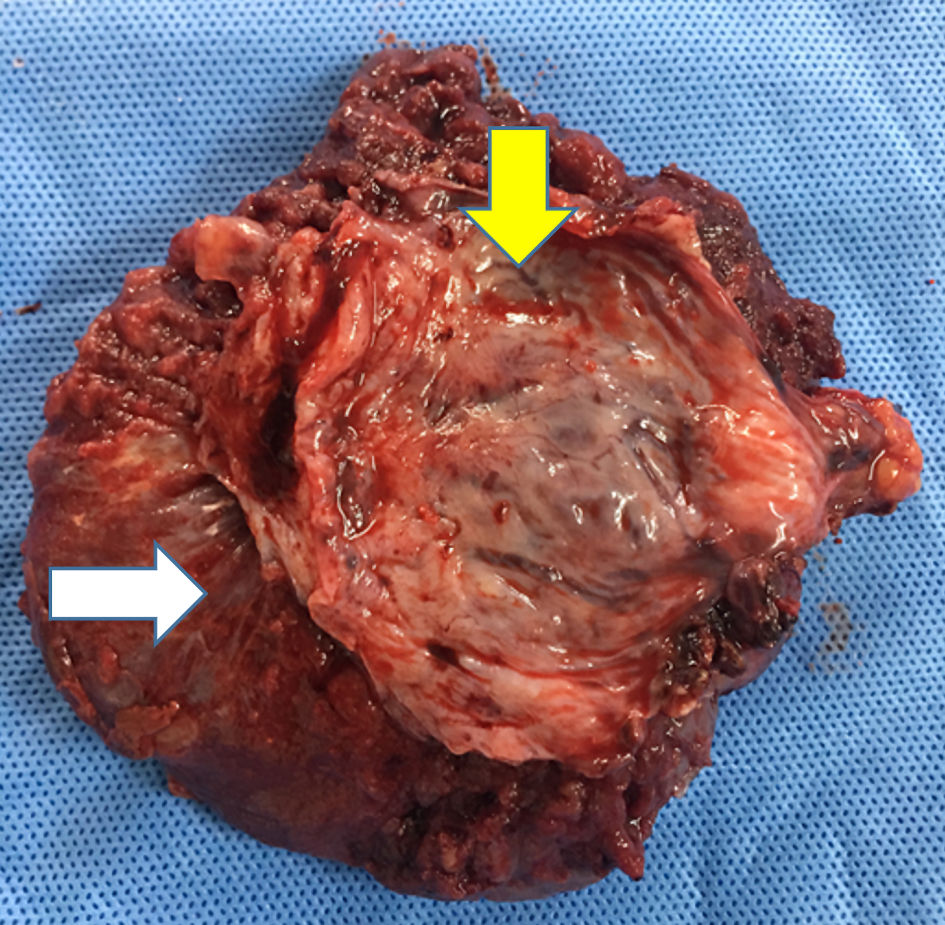
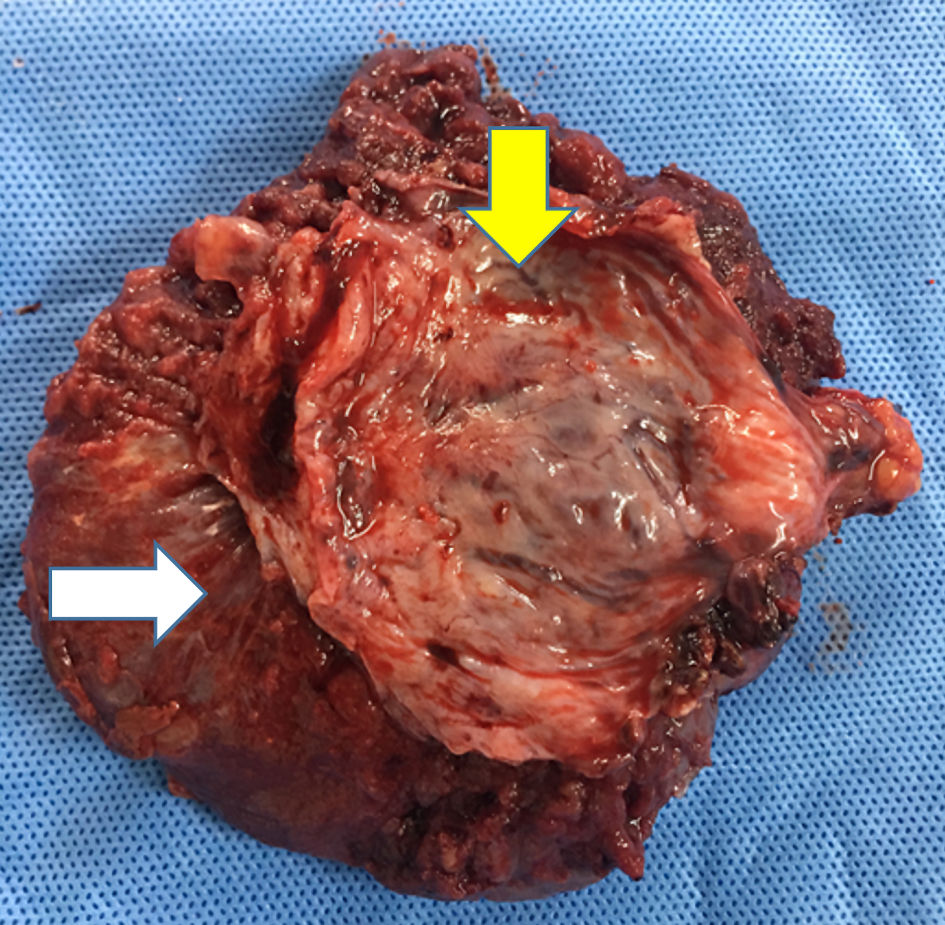
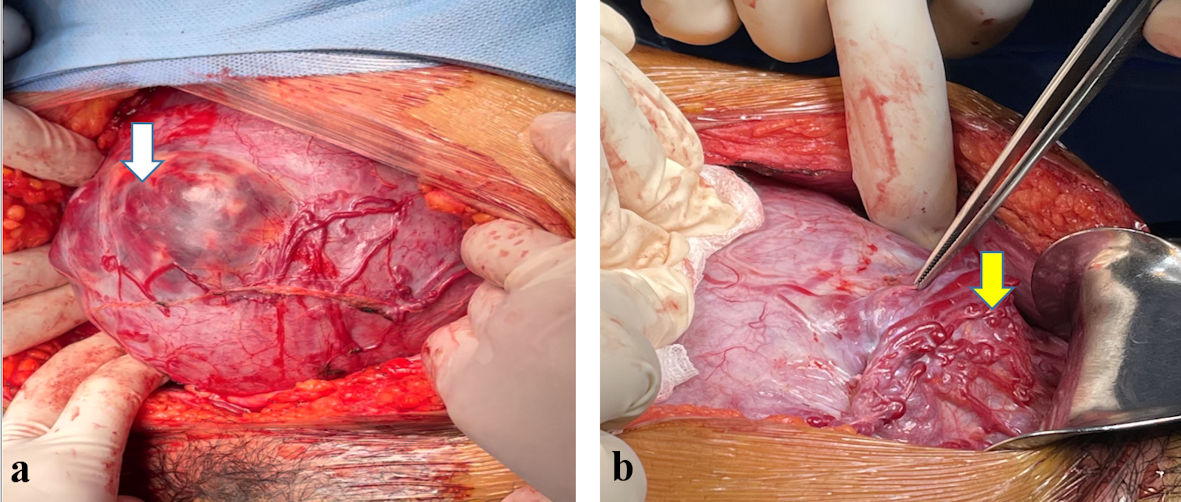
Figure 1. Myometrial part of uterus (yellow arrow) was removed accompanied with specimen of unseparated placenta (white arrow).
| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website https://www.jcgo.org |
Original Article
Volume 11, Number 3, September 2022, pages 75-85
A Novel Approach in Management of Placenta Accreta Spectrum Disorders: A Single-Center Surgical Experience From Vietnam
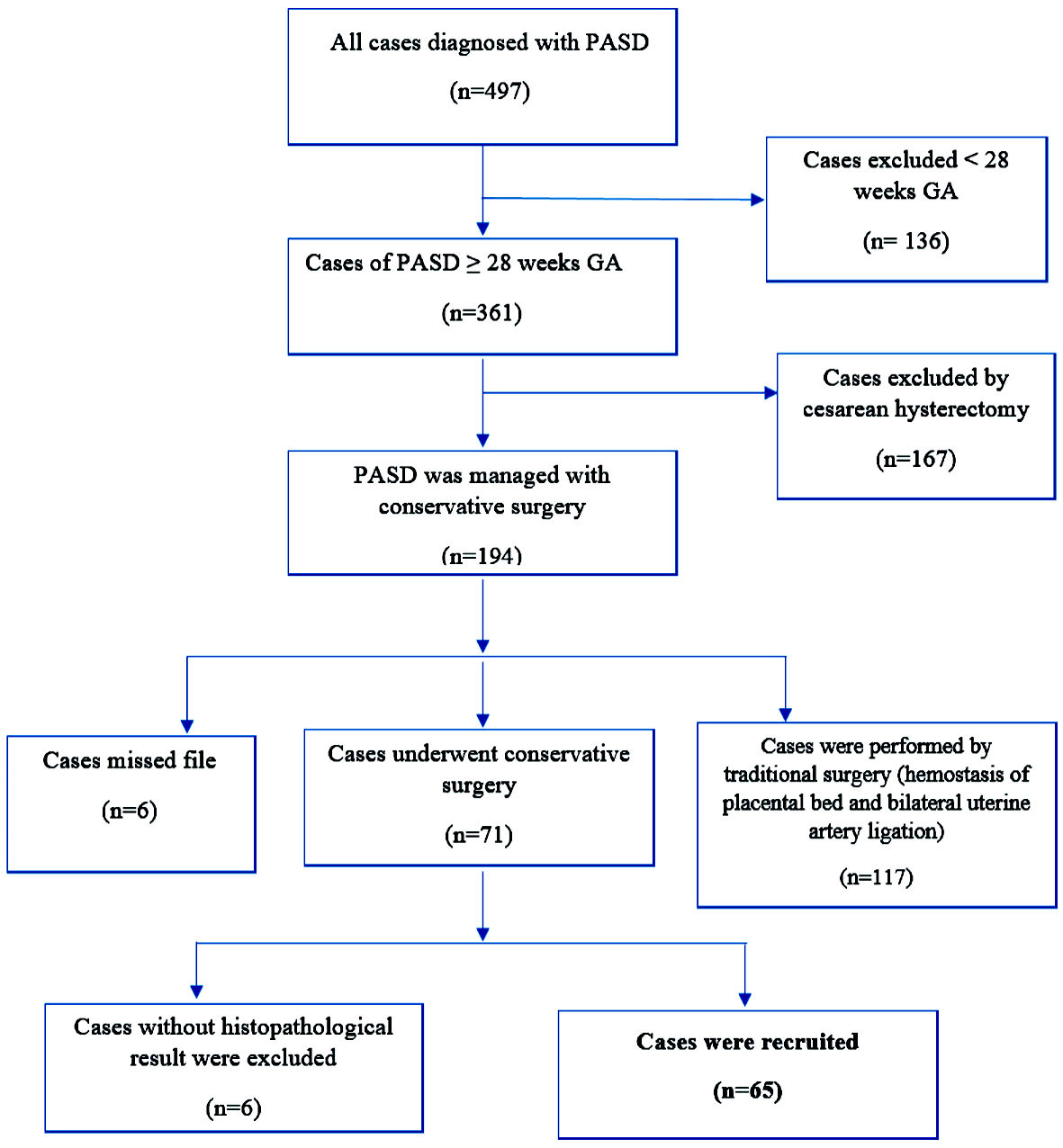
Figures
Tables
| Step 1: vascular disconnection of proliferative vessels and the separation of invaded uterine tissues from invaded vesical tissues. |
| Step 2: incision of the lower uterine segment at upper margin of placenta or cut through placenta, fetal delivery. |
| Step 3: resection of all invaded myometrial portion, manual removal of the whole placenta, or left partial placenta in situ, hemostasis of local bleeding vessels (Fig. 1). |
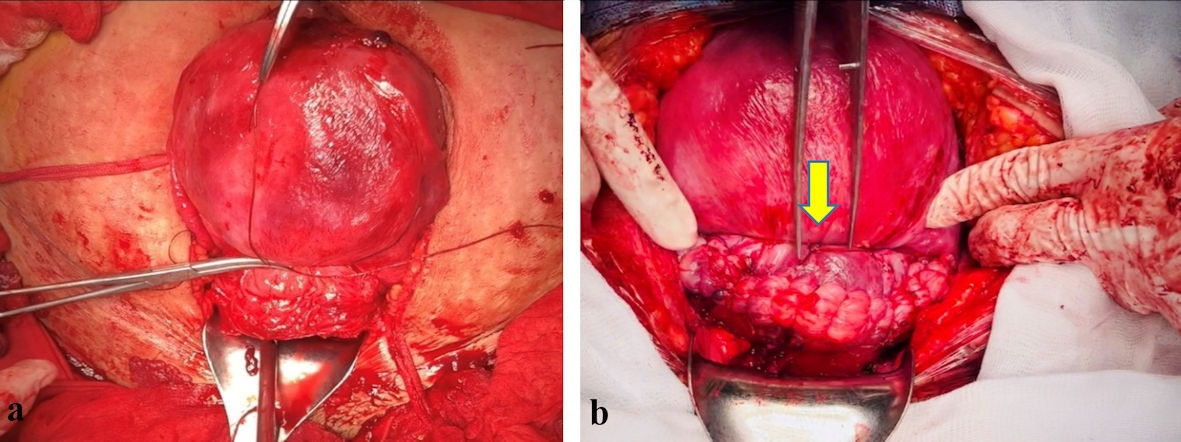
| Step 4: hemostasis by suture of transverse B-Lynch procedure (uterine compression suture), using atraumatic number 1 chromic catgut (Fig. 2a) [14]. |
| Step 5: restore of uterine myometrium by one layer, not using suture of “U” shape (Fig. 2b). |
| Step 6: bladder repair if necessary. |
| Features | Frequency (n) | Percentage (%) |
|---|---|---|
| SD: standard deviation. | ||
| Maternal age (mean ± SD) | 32.78 ± 5.19 | |
| < 35 | 39 | 60 |
| ≥ 35 | 26 | 40 |
| Number of previous cesarean scar | ||
| 0 | 3 | 4.6 |
| 1 | 38 | 58.5 |
| 2 | 23 | 35.4 |
| 3 | 1 | 1.5 |
| Gestational age at cesarean delivery (weeks) (mean ± SD) | 35.4 ± 2.1 | |
| 28+0 - 33+6 | 10 | 15.4 |
| ≥ 34+0 - 36+6 | 40 | 61.5 |
| ≥ 37+0 | 15 | 23.1 |
| Insertion of JJ catheter at cesarean delivery | ||
| Yes | 55 | 84.6 |
| No | 10 | 15.4 |
| Bilateral uterine artery ligation | ||
| Yes | 61 | 93.8 |
| No | 4 | 6.2 |
| Selective ligation of vescical-uterine vessels | ||
| Yes | 61 | 93.8 |
| No | 4 | 6.2 |
| Other hemostatic procedures | ||
| Yes | 14 | 21.5 |
| No | 51 | 78.5 |
| Intervention of bladder repair | ||
| Yes | 3 | 4.6 |
| No | 62 | 95.4 |
| Duration from skin incision to fetal delivery (min) mean ± SD | 30 ± 18.8 | |
| Left partial placenta in situ | 7 | |
| Newborn outcomes | Frequency (n = 65) | Percentage (%) |
|---|---|---|
| SD: standard deviation; NICU: neonatal intensive care unit; CPAP: continuous positive airway pressure; NIPPV: noninvasive positive pressure ventilation; ETT: endotracheal tube. | ||
| Weight of newborn infant | ||
| Mean ± SD | 2,466 ± 515 | |
| 1,000 - ≤ 1,500 g | 3 | 4.6 |
| >1,500 - ≤ 2,500 g | 35 | 53.9 |
| > 2,500 g | 27 | 41.5 |
| Apgar score at 1 min | ||
| Low (0 - 3) | 7 | 10.8 |
| Middle (4 - 6) | 55 | 84.6 |
| Normal (7 - 10) | 3 | 4.6 |
| Apgar score at 5 min | ||
| Middle (4 - 6) | 23 | 35.4 |
| Normal (7 - 10) | 42 | 64.6 |
| NICU | ||
| Yes | 40 | 61.5 |
| No | 24 | 36.9 |
| Delivery to tertiary neonatal hospital | 1 | 1.6 |
| Postnatal intervention | ||
| No need oxygen support | 13 | 20.0 |
| Oxygen via nasal cannula | 25 | 38.5 |
| CPAP | 15 | 23.1 |
| NIPPV | 5 | 7.7 |
| ETT | 7 | 10.8 |
| Infant status during postnatal course | ||
| Alive | 59 | 90.7 |
| Transferred to tertiary hospital | 6 | 9.3 |
| Death | 0 | 0 |
| Frequency (n = 65) | Percentage (%) | |
|---|---|---|
| aN = 57. SD: standard deviation. | ||
| Blood loss amount | ||
| Mean ± SD, mL | 987 (677 - 1,531) | |
| < 500 mL | 8 | 12.3 |
| Grade I, II (500 - < 1,500) mL | 43 | 66.2 |
| Grade III, IV (1,500 - < 3,000) mL | 11 | 16.9 |
| ≥ 3,000 mL | 3 | 4.6 |
| Ureteral injury (at stage of insertion of JJ catheter) | 1 | 1.5 |
| Tubal sterilization | 28 | 43.1 |
| Operation time | ||
| Mean ± SD, min | 135 ± 31.8 | |
| < 120 min | 22 | 33.8 |
| 120 - 180 min | 39 | 60.0 |
| > 180 min | 4 | 6.2 |
| Postoperative hemorrhage, relaparotomy with conservative management | 1 | 1.5 |
| Postoperative hemorrhage, relaparotomy with hysterectomy | 1 | 1.5 |
| Postoperative infection, medical therapy, no need of more surgical intervention | 2 | 3.1 |
| Postoperative infection, relaparotomy with hysterectomy | 2 | 3.1 |
| Postpartum course (days) | ||
| Mean ± SD | 5.79 (4.66 - 7.11) | |
| < 7 | 53 | 81.5 |
| 7 - ≤ 14 | 11 | 16.9 |
| > 14 | 1 | 1.5 |
| Blood transfusion volume (mL)a | ||
| Red blood cells | 831 ± 672 | |
| Fresh frozen plasma | 446 ± 158 | |
| Platelet | 250 | |
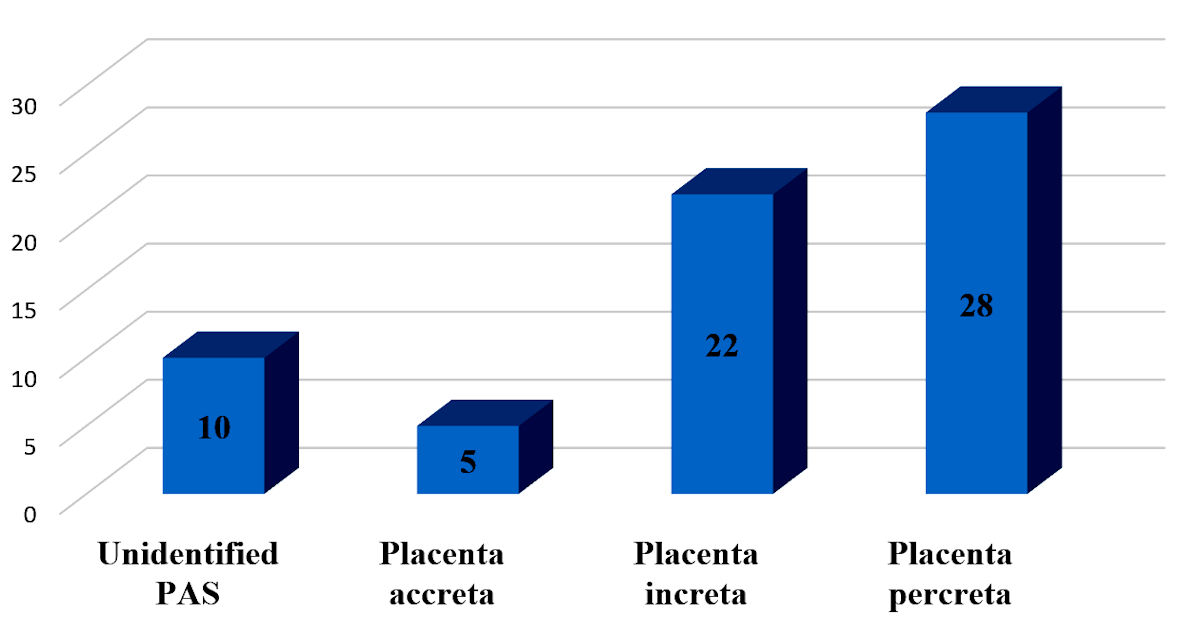
| Features | Histopathological result | ||||
|---|---|---|---|---|---|
| Unidentified PAS n (%) | Placenta accreta n (%) | Placenta increta n (%) | Placenta percreta n (%) | Total n (%) | |
| PAS: placenta accreta spectrum. | |||||
| Surgery | |||||
| Elective | 10 (16.9) | 4 (6.8) | 20 (33.9) | 25 (33.9) | 59 (100.0) |
| Emergency | 0 (0.0) | 1 (16.7) | 2 (33.3) | 3 (50.0) | 6 (100.0) |
| Blood loss amount | |||||
| < 1,500 mL | 9 (20.5) | 2 (4.5) | 15 (34.1) | 18 (40.9) | 44 (100.0) |
| ≥ 1,500 mL | 1 (4.8) | 3 (14.3) | 7 (33.30) | 10 (47.6) | 21 (100.0) |