| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website http://www.jcgo.org |
Case Report
Volume 3, Number 3, September 2014, pages 114-116
Are Monochorionic Twins More Likely Subsequent to Blastocyst Transfer? A Case Report and Experience With the “German Middle Way”
Ines Beyera, b, Dunja Baston-Busta, Andrea Schanza, Jan-Steffen Krussela, Alexandra Hessa
aDepartment of Obstetrics and Gynecology and REI (UniKiD), Medical Center University of Dusseldorf, Moorenstr. 5, Dusseldorf 40225, Germany
bCorresponding Author: Ines Beyer, Department of Obstetrics and Gynecology and REI (UniKiD), Medical Center University of Dusseldorf, Moorenstr. 5, Dusseldorf 40225, Germany
Manuscript accepted for publication August 11, 2014
Short title: Blastocyst Transfer
doi: https://doi.org/10.14740/jcgo274w
| Abstract | ▴Top |
Since the introduction of assisted reproductive techniques the amounts of monozygotic twins (MZTs) have been rising. Several studies have suggested that blastocyst culture and the associated prolonged in vitro cultivation time might play a role in the manifestation of monochorionic twins. Due to the recent changes in the interpretation of the German Embryo Protection Act, it became accepted for patients and doctors in some regions of Germany to select for the most suitable embryo prior to implantation, referred to as the “German middle way”. We report a rare case of two sets of monochorionic and diamniotic twins subsequent to blastocyst transfer. A missed abortion of one of the twin sets occurred at the eighth week of gestation. The ongoing pregnancy showed no further signs of pathology and two healthy twins were delivered per cesarean section at 38 weeks. This case demonstrates that patients should be well informed concerning the risk for monochorionic twins subsequent to blastocyst transfer. In our experience, however, blastocyst transfer on day 5 does not seem to increase the risk for monochorionic twins compared to in vitro fertilization (IVF)/intracytoplasmic sperm injection (ICSI) with transfer on day 2.
Keywords: Monochorionic twins; Blastocyst transfer; German middle way
| Introduction | ▴Top |
Monochorionic twins give rise to a high risk pregnancy, associated with a higher rate of perinatal and maternal complications. In about 10-20% of the cases, feto-fetal transfusion syndrome occurs, leading to severe problems [1]. The risk for monozygotic twins (MZTs) in the general population is as low as approximately 0.4% [2]. Since the introduction of assisted reproductive techniques the amounts of twins and MZTs have been rising [2]. Approximately 75% of all MZTs are monochorionic. Several studies have suggested that blastocyst culture and the associated prolonged in vitro cultivation time might play a role in the manifestation of monochorionic twins [3-6]. Due to the recent changes in the interpretation of the German Embryo Protection Act, it became accepted for patients and doctors in some regions of Germany to select for the most suitable embryo prior to implantation. It is now common practice to perform a blastocyst transfer of the best quality embryo (or embryos) out of a maximum of six fertilized oocytes yielded via prolonged cultivation and selection for the “most suitable”, referred to as the “German middle way” [7, 8]. We report a rare case of two monochorionic twin couples (dichorionic, quadramionic quadruplets) after transfer of two blastocysts in a patient after intracytoplasmic sperm injection (ICSI) therapy in light of our experience with MZT rate subsequent to blastocyst transfer.
| Case Report | ▴Top |
A 36-year-old nulligravida was referred to us with her 42-year-old partner due to unexplained infertility. The couple had tried to conceive for over 3.5 years prior to consulting us. The women had a mild form of endometriosis (ASRM Score I°) and a well treated Hashimoto’s thyreoiditis. She showed only mild peritoneal lesions of endometriosis and no other signs of pathology in a diagnostic laparoscopy. The patient had a regular menstrual cycle (29/3) and ultrasound of the female genital tract at day 3 of the cycle showed no abnormalities. Additionally the hormone profile showed values within the normal range for follicle-stimulating hormone (FSH), estradiol (E2), luteinizing hormone (LH), testosterone, prolactin, dehydroepiandrosterone (DHEA), dehydroepiandrosterone sulfate (DHEAS), thyroid-stimulating hormone (TSH), androstenedione and sex hormone-binding globulin (SHBG). Her partner was diagnosed with oligoasthenoteratozoospermia (OAT) syndrome III°. Therefore, an in vitro fertilization (IVF) combined with an ICSI was recommended. The patient was stimulated with the long agonist protocol with 0.2 mg/mL nafarelin and 150 international units of recombinant FSH for the first two cycles. In the third and fourth cycles additional human menopausal gonadotropin (HMG) injections, starting on stimulation day 8 and 6 respectively, were administered. In the first three cycles, two good quality embryos were transferred in each cycle after 2 days of culture, resulting in one pregnancy, which led to a missed abortion at the ninth week of gestation in the third cycle. In the fourth cycle we transferred two blastocysts after 5 days of culture (Fig. 1A). This transfer resulted in two monochorionic diamniotic twin pregnancies observed by ultrasound-scan investigation in the sixth week of gestation. In the eighth gestational week, ultrasound-scan revealed one ongoing intact monochorionic twin pregnancy and a missed abortion of the second twin pregnancy. At the 10th week of gestation the one monochorionic twin pregnancy developed normally (Fig. 1B). The first trimester screening and the organ screening at 20 weeks of gestation showed no pathology. Further development of the twins proceeded normally and showed no signs of feto-fetal transfusion syndrome or other complications. The pregnancy was electively terminated at 38 weeks of gestation and the healthy twins were delivered by cesarean section.
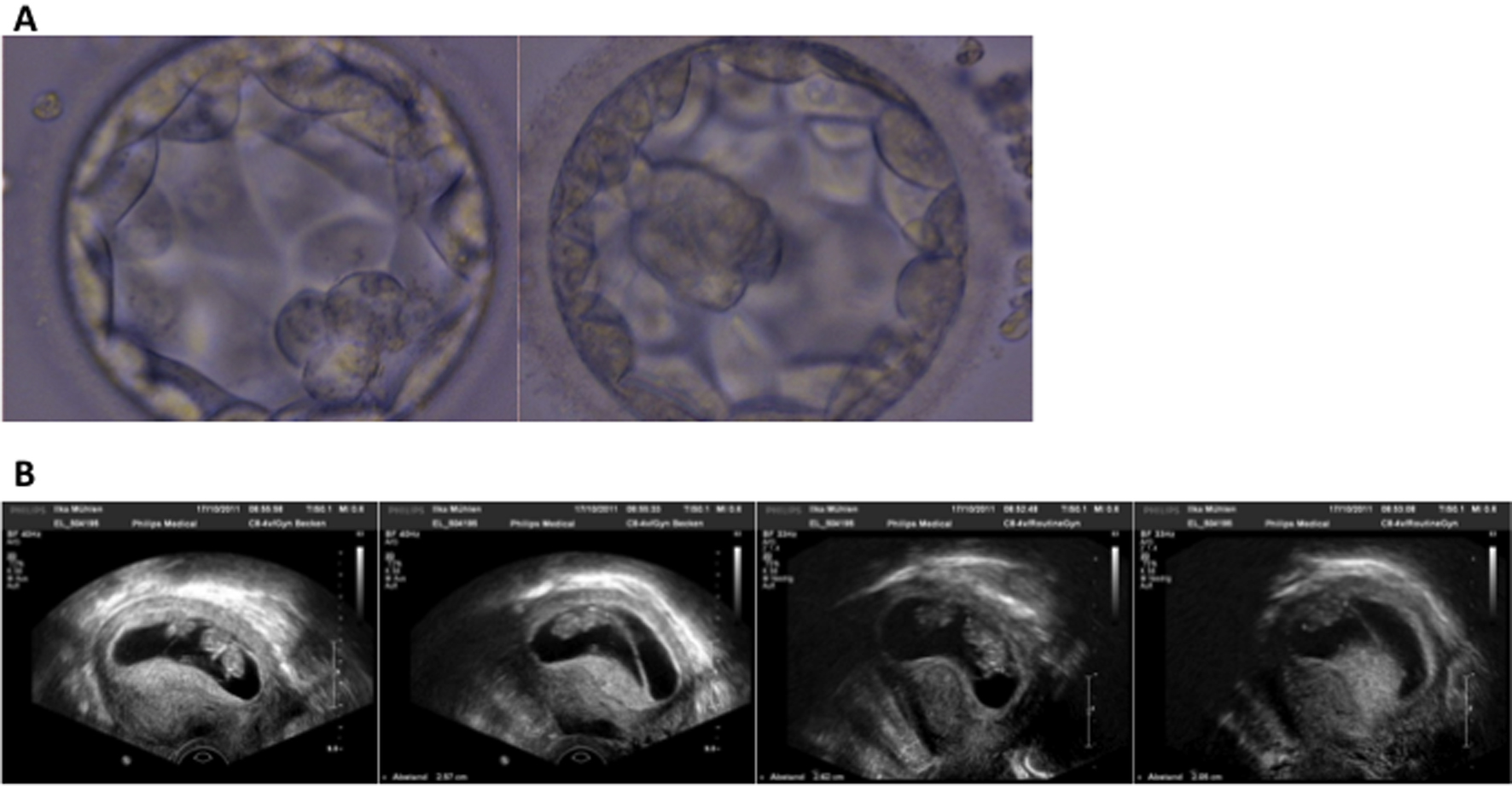 Click for large image | Figure 1. (A) Image of the blastocysts transferred on day 5 of in vitro culture. The ultrasound scan at the 10th week of gestation. (B) Showing the chorionicity. Showing the normal developed monochorionic twins. Showing the missed abortion of one twin pregnancy. |
| Discussion | ▴Top |
Although the selection for the best quality embryo and blastocyst transfer has for years been a common practice in many countries, the data on monozygotic rates through blastocyst transfer are not conclusive. The current opinion in the literature shows increased rates of MZTs, as well as a reduced risk factor after blastocyst transfer.
The question remains, however, if blastocyst transfer on day 5 of a single embryo elevates the MZT rate versus transfer of an embryo on day 2, or whether it is rather the culture conditions and not the culture time that has the most influences. Two studies in Japan from Kawachiya et al (2011) and Nakasuji et al (2014), an 8-year experience from Knopman et al (2010) at an IVF center in New York and a meta-analysis from Chang et al (2009) showed an increased risk for MZT after blastocyst transfer, while a study from Papanikolaou et al (2010) showed no increased risk for MZT subsequent to blastocyst transfer compared to single cleavage stage embryo transfer [3, 4, 9-11]. In addition, data from Moayeri et al (2007) showed a decrease of the MZT rate with blastocyst transfer in their 8-year experience at the Stanford Medical Center [12]. This was attributed to the gained experience over the time and the changes and improvements of culture conditions itself. To date, in our experience at the largest university fertility clinic in Germany, we have not seen an increase of MZT rates in our patients. With the “German middle way”, in some regions of Germany, we are finally able to provide patients with a selection of suitable embryo and blastocyst transfers, leading to an increased probability of a pregnancy. In our experience, since November 2011, we have had a pregnancy rate of 31.7% in the group of patients 35 years and older with the “German middle way” versus 22.13% with the traditional transfer on day 2. To date, we have also seen a higher overall twin rate (9.19% versus 5.83%), but no increased risk for monochorionic twins between single cleavage stage embryo transfer and blastocyst transfer. With increasing experience it should be possible to further reduce the number of embryos per transfer (currently 1.99 - 2.02 according to the German IVF Registry, 2012) [13]. We conclude that the “German middle way” seems to be a safe strategy for couples seeking assisted reproductive therapy with the potential for a higher success rate. However, it is important that patients should be counseled on the overall higher twin rate and the possible complications associated with blastocyst transfer. Furthermore additional studies on culture conditions of the embryo and MZT rate should be conducted.
| References | ▴Top |
- Rao A, Sairam S, Shehata H. Obstetric complications of twin pregnancies. Best Pract Res Clin Obstet Gynaecol. 2004;18(4):557-576.
doi pubmed - Aston KI, Peterson CM, Carrell DT. Monozygotic twinning associated with assisted reproductive technologies: a review. Reproduction. 2008;136(4):377-386.
doi pubmed - Chang HJ, Lee JR, Jee BC, Suh CS, Kim SH. Impact of blastocyst transfer on offspring sex ratio and the monozygotic twinning rate: a systematic review and meta-analysis. Fertil Steril. 2009;91(6):2381-2390.
doi pubmed - Kawachiya S, Bodri D, Shimada N, Kato K, Takehara Y, Kato O. Blastocyst culture is associated with an elevated incidence of monozygotic twinning after single embryo transfer. Fertil Steril. 2011;95(6):2140-2142.
doi pubmed - Menezo YJ, Sakkas D. Monozygotic twinning: is it related to apoptosis in the embryo? Hum Reprod. 2002;17(1):247-248.
doi - da Costa AA, Abdelmassih S, de Oliveira FG, Abdelmassih V, Abdelmassih R, Nagy ZP, Balmaceda JP. Monozygotic twins and transfer at the blastocyst stage after ICSI. Hum Reprod. 2001;16(2):333-336.
doi - Geisthovel F, Beier HM, Ochsner A, Frommel M, Taupitz J. A novel algorithm of ART in Germany based on an adequate interpretation of the German Embryo Protection Act (Deutsches Embryonenschutzgesetz, ESchG). Hum Reprod. 2007;22:505.
- Bals-Pratsch M, Dittrich R, Frommel M. Wandel in der Implementation des Deutschen Embryonenschutzgesetzes. J Reproduktionsmed Endokrinol. 2010;7:87-95.
- Nakasuji T, Saito H, Araki R, Nakaza A, Nakashima A, Kuwahara A, Ishihara O, et al. The incidence of monozygotic twinning in assisted reproductive technology: Analysis based on results from the 2010 Japanese ART national registry. J Assist Reprod Genet. 2014;31(7):803-807.
doi pubmed - Knopman J, Krey LC, Lee J, Fino ME, Novetsky AP, Noyes N. Monozygotic twinning: an eight-year experience at a large IVF center. Fertil Steril. 2010;94(2):502-510.
doi pubmed - Papanikolaou EG, Fatemi H, Venetis C, Donoso P, Kolibianakis E, Tournaye H, Tarlatzis B, et al. Monozygotic twinning is not increased after single blastocyst transfer compared with single cleavage-stage embryo transfer. Fertil Steril. 2010;93(2):592-597.
doi pubmed - Moayeri SE, Behr B, Lathi RB, Westphal LM, Milki AA. Risk of monozygotic twinning with blastocyst transfer decreases over time: an 8-year experience. Fertil Steril. 2007;87(5):1028-1032.
doi pubmed - Buhler K, Bals-Pratsch M, Blumenauer V, Dahncke W, Felberbaum R, Fiedler K, Gnoth C, Happel L, Krussel JS, Kupka MS, Wendelken M. DIR annual 2011. J Reproduktionsmed Endokrinol. 2012;9:453-484.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
