| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website http://www.jcgo.org |
Case Report
Volume 4, Number 1, March 2015, pages 193-196
A Problematic Peril of Pessaries: The Rare Case of Rectovaginal Fistulas Resulting From Pessary Use
Geoffrey H. Gordona, d, Thomas F. Dolnicekb, Vinay K. Malviyac
aDepartment of Obstetrics and Gynecology, Providence Hospital, 16001 West 9 Mile Rd, Southfield, MI 48075, USA
bDivision of Female Pelvic Medicine and Reconstructive Surgery, Department of Obstetrics and Gynecology, Providence Hospital, 16001 West 9 Mile Rd, Southfield, MI 48075, USA
cDivision of Gynecologic Oncology, Department of Obstetrics and Gynecology, Providence Hospital,16001 West 9 Mile Rd, Southfield, MI 48075, USA
dCorresponding Author: Geoffrey H. Gordon, Department of Obstetrics and Gynecology, Providence Hospital, 16001 West 9 Mile Rd, Southfield, MI 48075, USA
Manuscript accepted for publication February 03, 2015
Short title: Rectovaginal Fistulas
doi: http://dx.doi.org/10.14740/jcgo308w
| Abstract | ▴Top |
Pelvic organ prolapse (POP) is a condition of herniation of the pelvic organs into the vagina or past the introitus. Management options include pessary use. A very rare complication of pessary usage is erosion resulting in a vesicovaginal or rectovaginal fistula. We present two cases of patients who were found to have rectovaginal fistulas from Gellhorn pessary usage. Both patients were surgically treated with colostomies. Pessary management of POP is very common and accepted form of treatment. For optimal outcomes with pessary use, we recommend that patients be actively managed with individualized periodic evaluations. Estrogen cream may be considered for prevention and treatment of eroded vaginal epithelium.
Keywords: Pessary; Rectovaginal fistula
| Introduction | ▴Top |
Pelvic organ prolapse (POP) is a common finding on physical exam [1]. However, the degree of POP, as well as the symptoms, can be highly variable among patients. Exact epidemiological data for prevalence of POP are lacking in current literature. The estimated prevalence ranges from 3% to 6% based on symptoms and up to 50% based on vaginal exam [2]. The number of surgical interventions to correct POP for women over 50 years old is 2.7 - 3.3 per 1,000 women [3]. Nonsurgical management of POP may be achieved by use of a pessary. The pessary is a foreign object in constant contact with the vaginal epithelium, therefore, its use requires that the patient have adequate follow-up to ensure proper fitting and integrity of the vaginal epithelium. Complications of pessary use include vaginal discharge and bleeding. Rarely, fistula formation, either vesicovaginal or rectovaginal, has been reported. The documented literature on fistulas resulting from pessary use is minimal and therefore lacks a standardized protocol for management. We present two cases of rectovaginal fistulas from our institution and discuss the possible management options for repair.
| Case Reports | ▴Top |
Case 1
An 88-year-old G3P3 (three full-term vaginal deliveries) Caucasian female with dementia was brought from her nursing care facility to the Emergency Department with abdominal pain. Due to her dementia, the history was obtained from her son. The patient had been seen at another hospital several times for the same complaint and was only diagnosed with constipation. Her medical history included carotid vascular disease, hypertension, peripheral vascular disease, and two strokes. Her surgical history was negative. On exam, her abdomen was distended and firm with bowel sounds auscultated. There was no guarding or rebound appreciated. Her vital signs were stable. Her complete blood count and basic metabolic panel were normal. Following a rectal enema for her constipation, stool was noted per vagina and a gynecology consult was placed. A CT scan (Fig. 1) was also ordered at that time which revealed severe fecal impaction, an over distended bladder, and a Gellhorn pessary. On gynecologic exam, the Gellhorn pessary stem was palpated vaginally and the posterior vaginal epithelium encircling the pessary stem was noted to be indurated. Rectal exam revealed the pessary dish to be at an oblique angle, blocking the lumen of the rectum, with only about a centimeter of space between the pessary and the sacral promontory. This finding let to further questioning of the patient’s son which revealed a history of POP and pessary placement. The son thought that the pessary had been taken out a few years earlier. The patient was admitted to our gynecologic oncology service and consent was obtained through her son for manual fecal disimpaction, pessary removal, and creation of a loop colostomy for subsequent stool management.
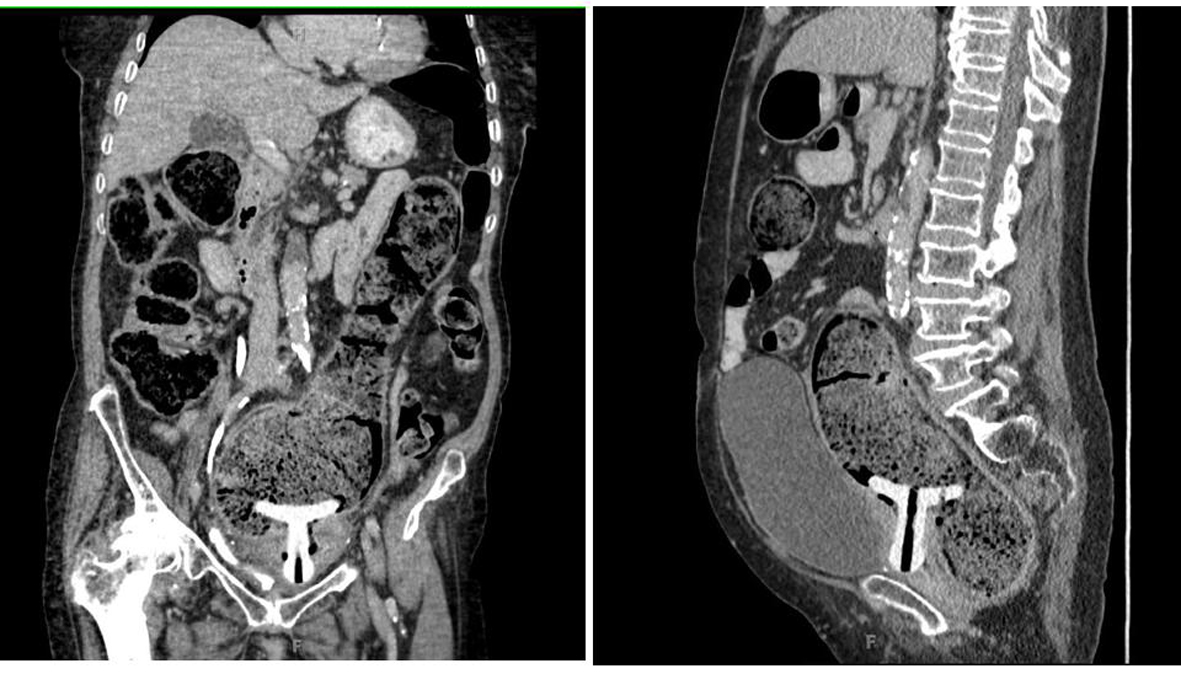 Click for large image | Figure 1. Sagittal and coronal CT images demonstrating a Gellhorn pessary situated in the vagina and the rectum. |
In the operating room the pessary was removed transrectally. The distended colon was palpable through the abdominal wall. The descending colon was massaged transabdominally and the stool was disimpacted via the rectum. A mini-laparotomy was then performed with the incision placed approximately 5 cm to the right of the umbilicus. A diverting loop colostomy from a segment of the descending colon was successfully created. Due to the poor quality of the vaginal tissue, no attempt was made to close the fistula. Post-operatively, the patient had slow post-operative return of bowel function and was discharged after 11 days with appropriate colostomy function and stable return to baseline function. She was discharged to a nursing facility for further rehabilitation. At the most recent follow-up, the patient had developed a stricture of her colostomy, which is functional. On physical exam, the fistulous communication has healed.
Case 2
A 64-year-old G3P2012, with a history of two full-term vaginal deliveries, was evaluated by her gynecologist in consultation from the Internal Medicine team for urinary retention secondary to POP. She was hospitalized on the Internal Medicine service for urinary sepsis and renal failure. She had an extensive medical history of a recent myocardial infarction, hypertension, insulin dependent diabetes mellitus, coronary artery disease, peripheral vascular disease, dyslipidemia, anemia, and arthritis. A previous attempt at pessary management was unsuccessful when the pessary fell out after 8 weeks of placement. On physical exam, complete procidentia that extended 7 - 8 cm past the introitus was noted, along with significant vaginal mucosal ulcerations that were bleeding. The prolapsed vagina was extensively coated with vaginal estrogen cream prior to pessary fitting attempts. The procidentia was unable to be reduced with a single pessary because of the chronically distended introitus. A space-occupying donut pessary was initially inserted, followed by the addition of a Gellhorn pessary. This combination of pessaries relieved her prolapsed and the associated pain. Her urinary sepsis and renal failure were successfully managed and the prolapse reduction allowed the medical team to optimize the medical management of her other multiple comorbidities. When her indwelling catheter was eventually able to be removed, she demonstrated urinary incontinence. Plans were made for outpatient management of her pessaries and prolapse until her medical team cleared her for ultimate operative repair.
Management of multiple comorbidities included hyperbaric oxygen therapy for severely MRSA infected lower limb ulcers secondary to peripheral vascular disease and coronary artery stenting performed for coronary artery disease, which prevented surgical intervention for 14 months. She was seen monthly by the gynecologist for pessary management. During that time, she complained of episodes of watery bloody discharge, which was felt to be secondary to vaginal mucosal epithelial ulcerations that were poorly healing because of pessary mechanical pressure and the same poor vascular disease complicating her limbs and heart. Attempted trials of pessary free intervals resulted in the immediate return of the painful prolapse, urinary retention, and urosepsis. Only a few pessary free days were achieved before reinsertion was required for medical indications and pain relief. This cycle was maintained during the long treatment of her comorbidities, until medical clearance was finally given for her planned Leforte colpocleisis. Urodynamic testing was performed during this time which revealed occult stress urinary incontinence (SUI). A transobturator suburethral sling procedure was planned for her incontinence. Her final office pessary management visit was 2 weeks prior to her operation. When the pessaries were removed in the operating room, interval development of a 1.5 - 2 cm rectovaginal fistula was noted. Tissue quality was judged to be too poor for primary fistula closure by the attending gynecologist. An interoperative colorectal surgery consult was obtained. The colorectal surgeon and a second gynecologist consultant agreed with that assessment and recommended a colostomy for stool diversion and management. No pessaries were reinserted. Two days later, the colorectal surgeon performed a laproscopic Hartmann colostomy.
The patient’s fistula improved over the next 3 months, became smaller, but it did not resolve. Her prolapse immediately returned post-operatively and continued to be painful, while the excessive watery, bloody discharge remained a management problem and contributed to her chronic anemia, requiring transfusion. The patient strongly requested another attempt at surgical management of her almost intolerable prolapsed. Her continued multiple medical comorbidities led the colorectal surgeon to recommend against rectovaginal fistula closure. The persistent rectovaginal fistula, located 3 cm from the introitus, precluded performance of the previously planned Leforte colpocleisis. A total vaginal hysterectomy and bilateral uterosacral ligament colpopexy were recommended to the patient for her prolapse and a TVT-O for her stress incontinence. When medical clearance was again obtained, these procedures were successfully performed.
The patient has achieved a significantly improved quality of life. She no longer has the large painful procidentia and the mechanical problems it caused. Her watery, bloody discharge has resolved. She enjoys urinary continence, but does suffer from recurrent urinary tract infections and occasional urgency. Her colostomy is functioning well and she currently is satisfied with colostomy management and does not desire further surgical procedures.
| Discussion | ▴Top |
The use of pessaries is an acceptable nonsurgical management option for patients with POP. However, patient selection and follow-up are a necessity to ensure successful and safe treatment. POP is often seen in postmenopausal patients where vaginal epithelium may be poorly estrogenized, which may put them at an increased risk for erosions from pessary use. Therefore, periodic visits to the gynecologist for assessment of vaginal epithelial integrity are often advised. These areas of epithelial breakdown may be treated with conjugated vaginal estrogen cream, silver nitrate local cauterization, or application of topical lubricant jellies recommended by the pessary manufacturer.
The risk for major complication such as fistula formation from pessaries is believed to be low, but this may be due to under reporting in the literature. An extensive literature search revealed a total of eight reported cases of recto-vaginal fistulas secondary to pessary usage [4-10]. The age range for the reported cases was 70 - 88 years old. Of interesting note, almost all of the reported cases in the literature were associated with the use of either a Gellhorn or shelf pessary. A possible cause of fistula formation following the use of a pessary could be due to a poorly fit pessary that may cause excessive mechanical force on the adjacent tissue and lead to erosion. It is possible that the general structure and design of the shelf and Gellhorn pessary, causes a disproportionate amount of pressure at the stem/dish into the vaginal wall leading to an increase in the risk of anterior and posterior wall erosions. Prolonged unattended pessaries also are at increased risk of fistula formation.
Management of rectovaginal fistulas associated with pessary management has been infrequently reported. Surgical management is frequently recommended and undertaken. Management of a diverting loop colostomy has been documented in two other cases [4, 5] and was planned in a third where the patient was lost for follow-up prior to surgery [6]. Other reported surgical methods of management include transvaginal repair with a graft [7], transperineal repair [8], and transrectal repair, which subsequently failed [9]. Most recently, Cichowski and Rogers [10] reported a patient who declined surgical repair of a rectovaginal fistula and achieved successful resolution by conservative management with estrogen cream. Though this nonsurgical approach with estrogen cream was successful, it may not be an ideal primary option for most patients. However, we do believe that intravaginal estrogen cream may prove to be a good adjuvant treatment along with surgical intervention in the resolution of rectovaginal fistula formation.
Our selection for the colostomy (loop or end) was based on the patients’ existing and overriding comorbidities. In the first case, our patient had severe fecal impaction with marked distention of bowels and poor mental status which contributed to an inability to perform activities of daily living. Her fistula formation is unique in that the dish of the pessary eroded into the rectum, whereas the previous case reports have noted fistula formation by erosion of the stem. On follow-up, our patient’s ostomy was functioning and her abdominal pain was resolved. The patient is mostly confined to bed and no longer finds her prolapse to be a concern. In the second case, our patient’s multiple medical problems contributed to her poor tissue quality as well as affecting her activities of daily living. On follow-up, there was dramatic improvement of her quality of life, including her urinary continence. She had significant decrease in the fistula size (1 cm diameter) and good support of the vaginal vault. Neither of our patients desired further surgical attempts at closure of their rectovaginal fistula.
There are no accepted guidelines for correcting rectovaginal fistulas secondary to pessary use. From our recent experience and following an extensive review of current literature we suggest that when faced with this dilemma, the management should be made on a case-by-case basis taking into account factors such as age, comorbidities, mental status, compliance, quality of vaginal tissue, patient desires, and size of the fistula (Fig. 2). We also believe that estrogen cream may augment the healing process. The benefit of a colostomy for treatment of rectovaginal fistulas caused by pessary use is the diversion of stool away from the healing vaginal fistula, allowing the optimum opportunity for spontaneous resolution of the fistula and application of local estrogen therapy if desired. Subsequent surgical fistula closure, if desired by the patient, can be performed when medical and tissue factor issues are optimized.
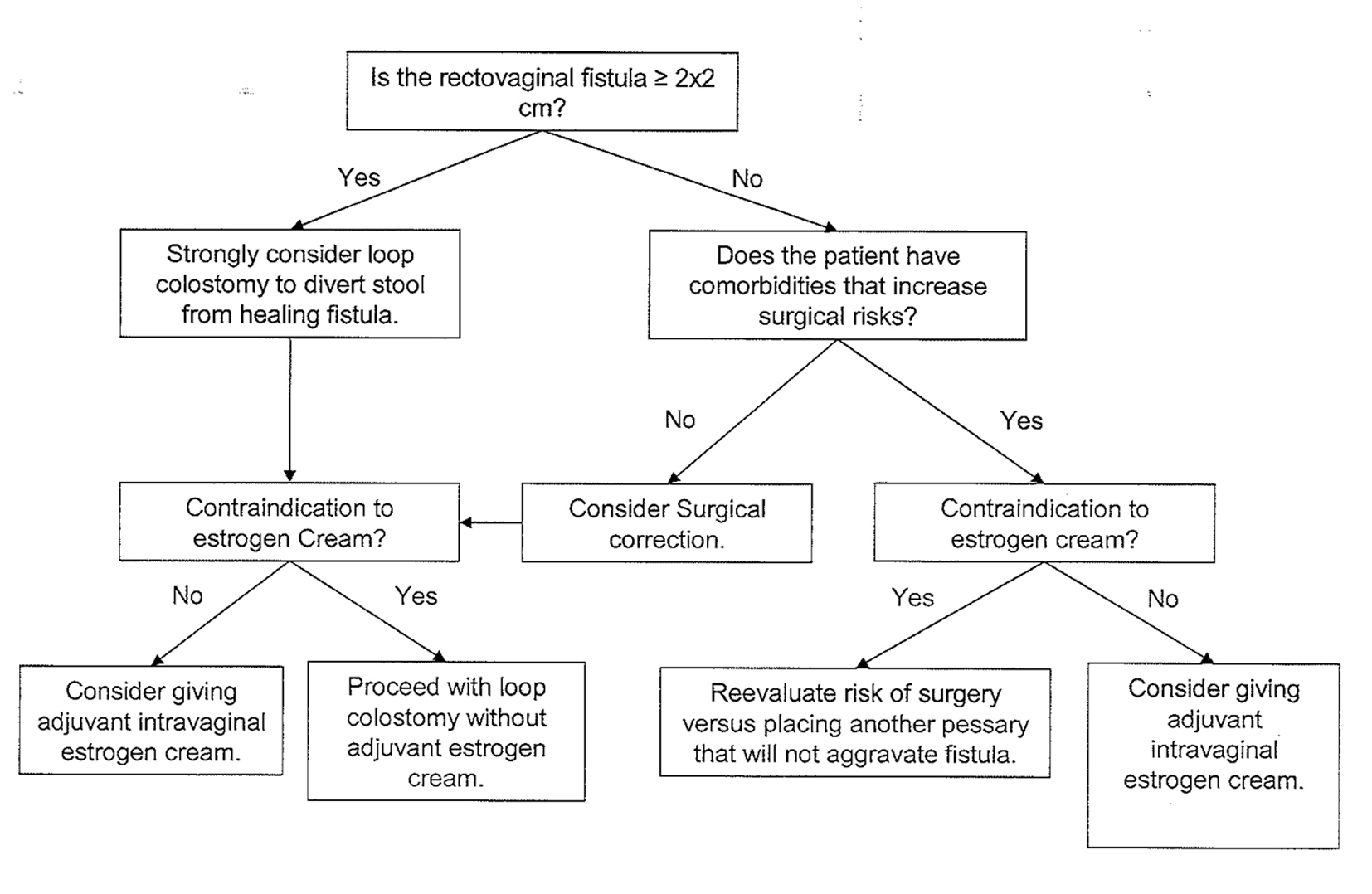 Click for large image | Figure 2. Algorithm of management of a rectovaginal fistula caused by pessary use. |
In summary, for optimal outcomes with pessary use, we recommend that patients be actively managed with individualized periodic evaluations. Estrogen cream may be considered for prevention and treatment of eroded vaginal epithelium.
Financial Disclosure
Authors report no financial disclosures.
| References | ▴Top |
- Swift SE. The distribution of pelvic organ support in a population of female subjects seen for routine gynecologic health care. Am J Obstet Gynecol. 2000;183(2):277-285.
doi pubmed - Barber MD, Maher C. Epidemiology and outcome assessment of pelvic organ prolapse. Int Urogynecol J. 2013;24(11):1783-1790.
doi pubmed - Boyles SH, Weber AM, Meyn L. Procedures for pelvic organ prolapse in the United States, 1979-1997. Am J Obstet Gynecol. 2003;188(1):108-115.
doi pubmed - Hanavadi S, Durham-Hall A, Oke T, Aston N. Forgotten vaginal pessary eroding into rectum. Ann R Coll Surg Engl. 2004;86(6):W18-19.
doi pubmed - Russell JK. The dangerous vaginal pessary. Br Med J. 1961;2(5267):1595-1597.
doi pubmed - Powers K, Grigorescu B, Lazarou G, Greston WM, Weber T. Neglected pessary causing a rectovaginal fistula: a case report. J Reprod Med. 2008;53(3):235-237.
pubmed - Yong PJ, Garrey MM, Geoffrion R. Transvaginal repair and graft interposition for rectovaginal fistula due to a neglected pessary: case report and review of the literature. Female Pelvic Med Reconstr Surg. 2011;17(4):195-197.
doi pubmed - Tarr M, Culbertson S, Lengyel E. Transverse Transperineal Repair of a Pessary-induced Mid-rectovaginal Fistula. 2008;14(3):199-201.
doi - Kankam OK, Geraghty R. An erosive pessary. J R Soc Med. 2002;95(10):507.
doi - Cichowski S, Rogers RG. Nonsurgical management of a rectovaginal fistula caused by a Gellhorn pessary. Obstet Gynecol. 2013;122(2 Pt 2):446-449.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
