| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website http://www.jcgo.org |
Case Report
Volume 4, Number 4, December 2015, pages 307-311
Heterotopic Cervical Pregnancy
Mathangi Thangavelua, b, Ravinder Kalkata
aGood Hope Hospital, Rectory Road, Sutton Coldfield B75 7RR, UK
bCorresponding Author: Mathangi Thangavelu, Good Hope Hospital, Rectory Road, Sutton Coldfield B75 7RR, UK
Manuscript accepted for publication October 26, 2015
Short title: Heterotopic Cervical Pregnancy
doi: http://dx.doi.org/10.14740/jcgo369w
| Abstract | ▴Top |
We report a rare case of heterotopic cervical pregnancy, which posed diagnostic challenge. With increasing IVF treatment and raising cesarean section rate, there is increasing incidence for non-tubal heterotopic pregnancy. We have discussed the clinical course of our case, diagnosis and management of cervical pregnancy and some good medical practices to avoid missing atypical presentations of ectopic pregnancy.
Keywords: Cervical pregnancy; Heterotopic; Ectopic
| Introduction | ▴Top |
We report an extremely rare case of spontaneous heterotopic cervical pregnancy who needed multiple investigations before the diagnosis of cervical pregnancy was made. This lady presented initially with symptoms of miscarriage and later was thought to have persistent trophoblastic disease before the final diagnosis of co-existing cervical pregnancy was made. Our case demonstrates the importance of scanning all atypical sites of ectopic even when there is evidence of intrauterine pregnancy on ultrasound.
| Case Report | ▴Top |
A 36-year-old nulliparous lady presented with a history of 7-week amenorrhoea and vaginal bleeding without any significant abdominal pain. She did not have any high risk factors for ectopic pregnancy. Speculum examination revealed some vaginal bleeding, cervix looked normal and cervical os was closed. On bimanual examination, there was no adnexal tenderness or cervical excitation. Initial hormonal investigations showed BHCG levels were raised to 17,276 IU and initial ultrasound was suggestive of minimal retained products of conception (Fig. 1). However, a repeat BHCG showed an increasing trend reaching up to 29,971 IU in 96 h. A repeat transvaginal scan showed the endometrial cavity had mixed echoes and multiple cystic spaces, largest measuring 6 × 7 × 8 mm with color flow suggesting a possible molar pregnancy (Fig. 2). Bilateral ovarian cysts were present in both adnexa.
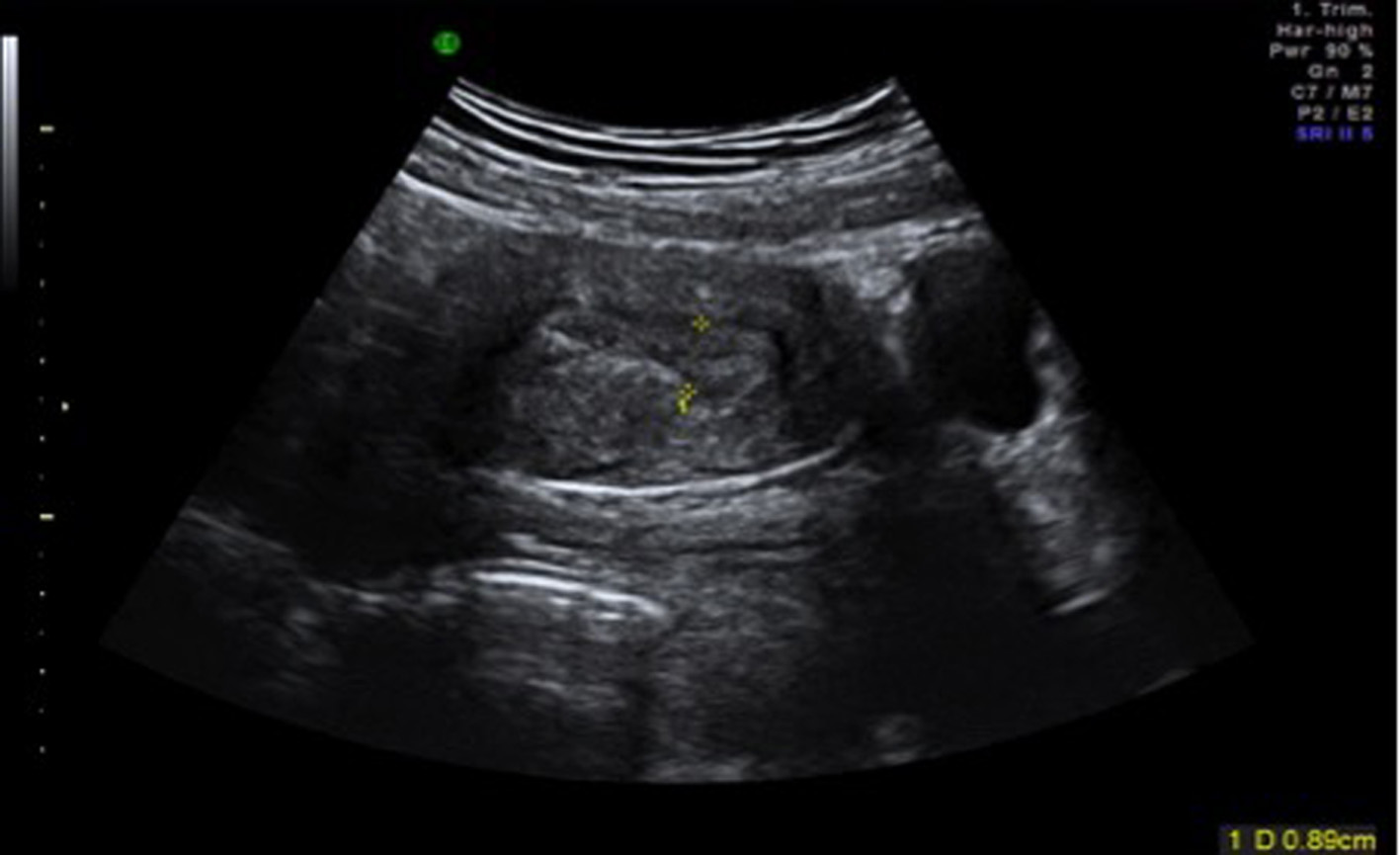 Click for large image | Figure 1. Initial transabdominal scan showing possible retained products of conception. |
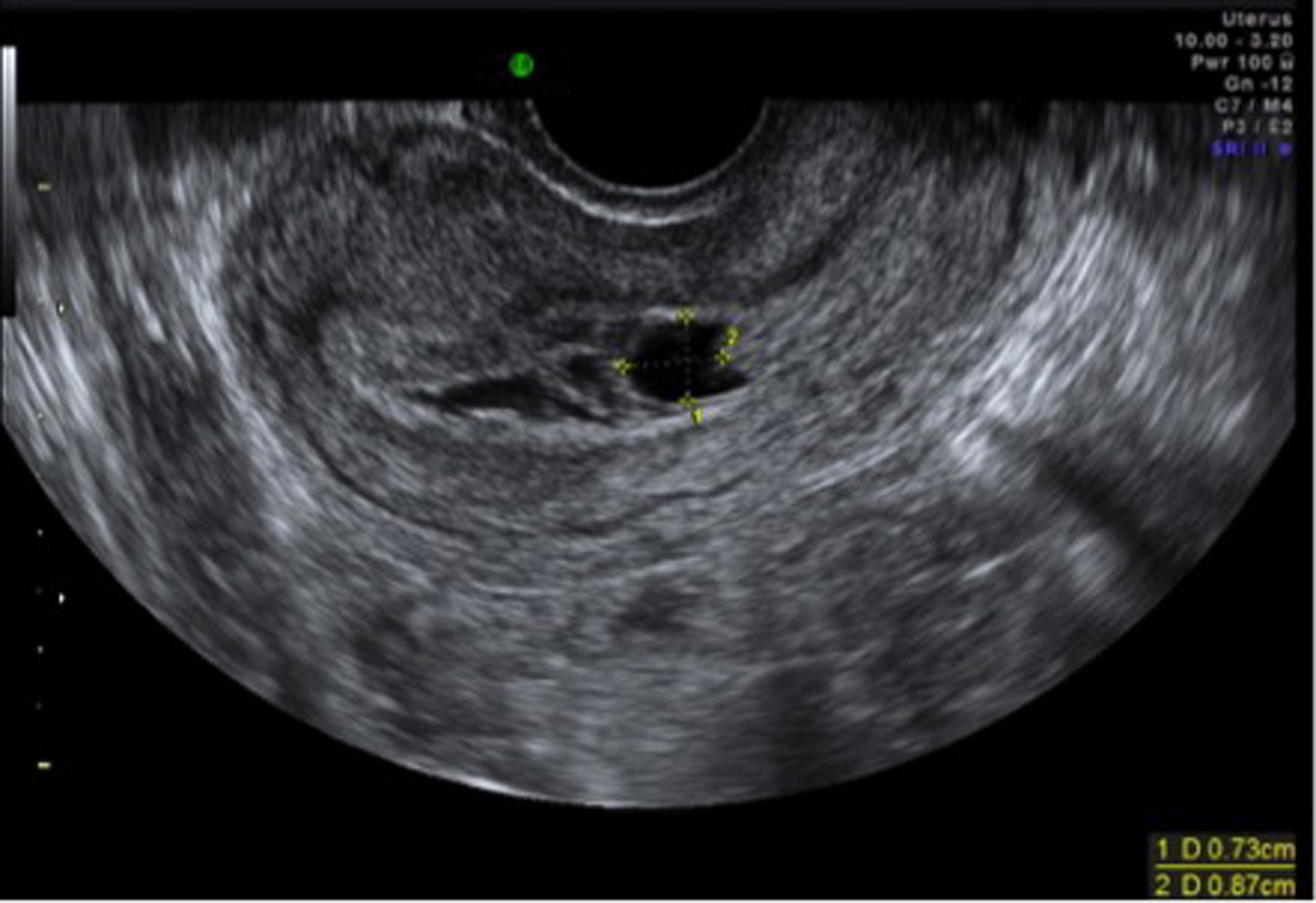 Click for large image | Figure 2. TV scan showing multiple cystic spaces suggesting possible molar pregnancy. |
Laparoscopy and dilatation and curettage were arranged in view of high BHCG levels and no clear evidence of intrauterine pregnancy. Laparoscopy was negative for tubal ectopic pregnancy and dilatation and curettage was performed. Postoperatively BHCG levels were monitored to ensure its levels were declining. The levels initially dropped to 2,611 IU from 29,971 IU in a week after D&C. However, the subsequent BHCG levels doubled to 4,207 IU 2 weeks after D&C. With the knowledge of earlier scan findings, raising BHCG levels raised the concern of persistent trophoblastic disease. However, the histology did not show any evidence of gestational trophoblastic disease. Patient remained asymptomatic apart from occasional bleed.
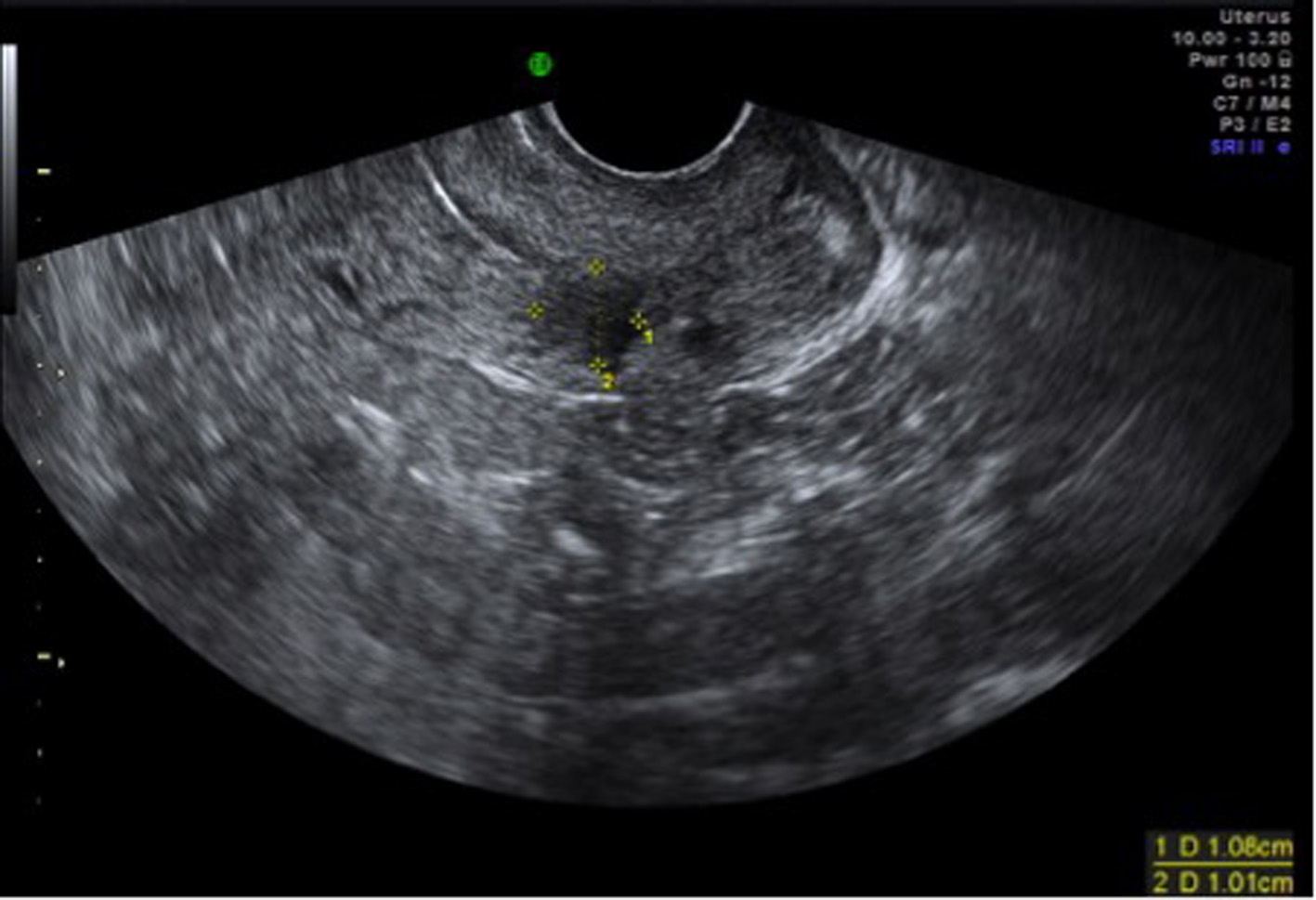
A repeat transvaginal ultrasound showed a hypoechoic area (gestational sac) with a possible fetal pole with a heterogenic area above the sac within the posterior wall of the cervix (Fig. 3, 4), raising the possibility of cervical ectopic pregnancy or retained products of conception low in the cervix. However, hysteroscopy showed a normal uterine cavity and no pregnancy tissues were identified in the cervical canal, suggesting cervical pregnancy was embedded in cervical musculature and any intra-cervical contents might have been removed during D&C performed earlier. A repeat suction evacuation was done but this had no effect on the increasing trend of BHCG, which increased to 4,832 IU. Methotrexate single dose injection was given and BHCG levels finally dropped to 17 IU over a period of 4 weeks. Repeat scan in 6 weeks showed resolution of gestational sac; however, surrounding heterogenic area did not resolve (Fig. 5).
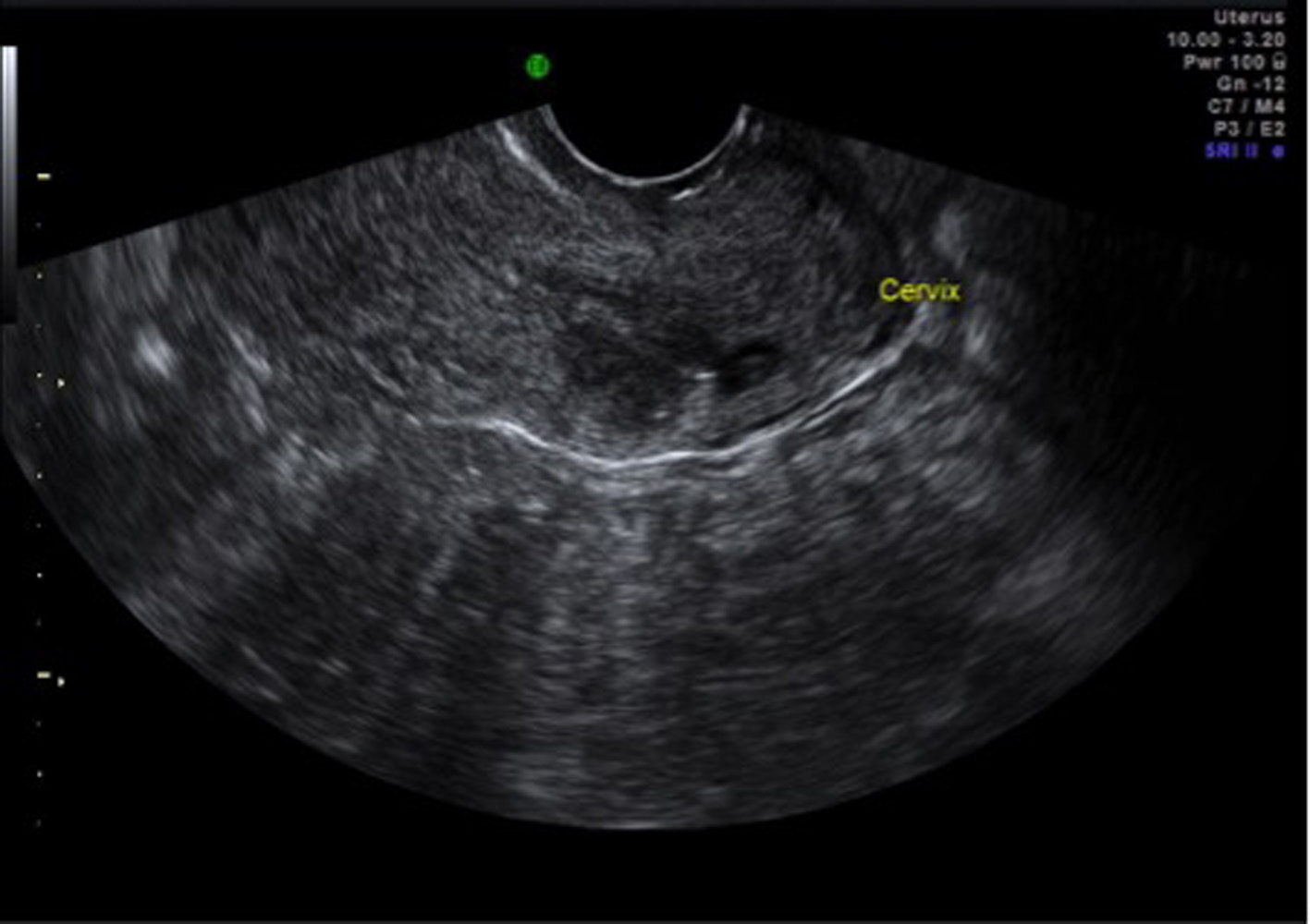 Click for large image | Figure 3. TV scan showing gestational sac and fetal pole in the posterior wall of cervix. |
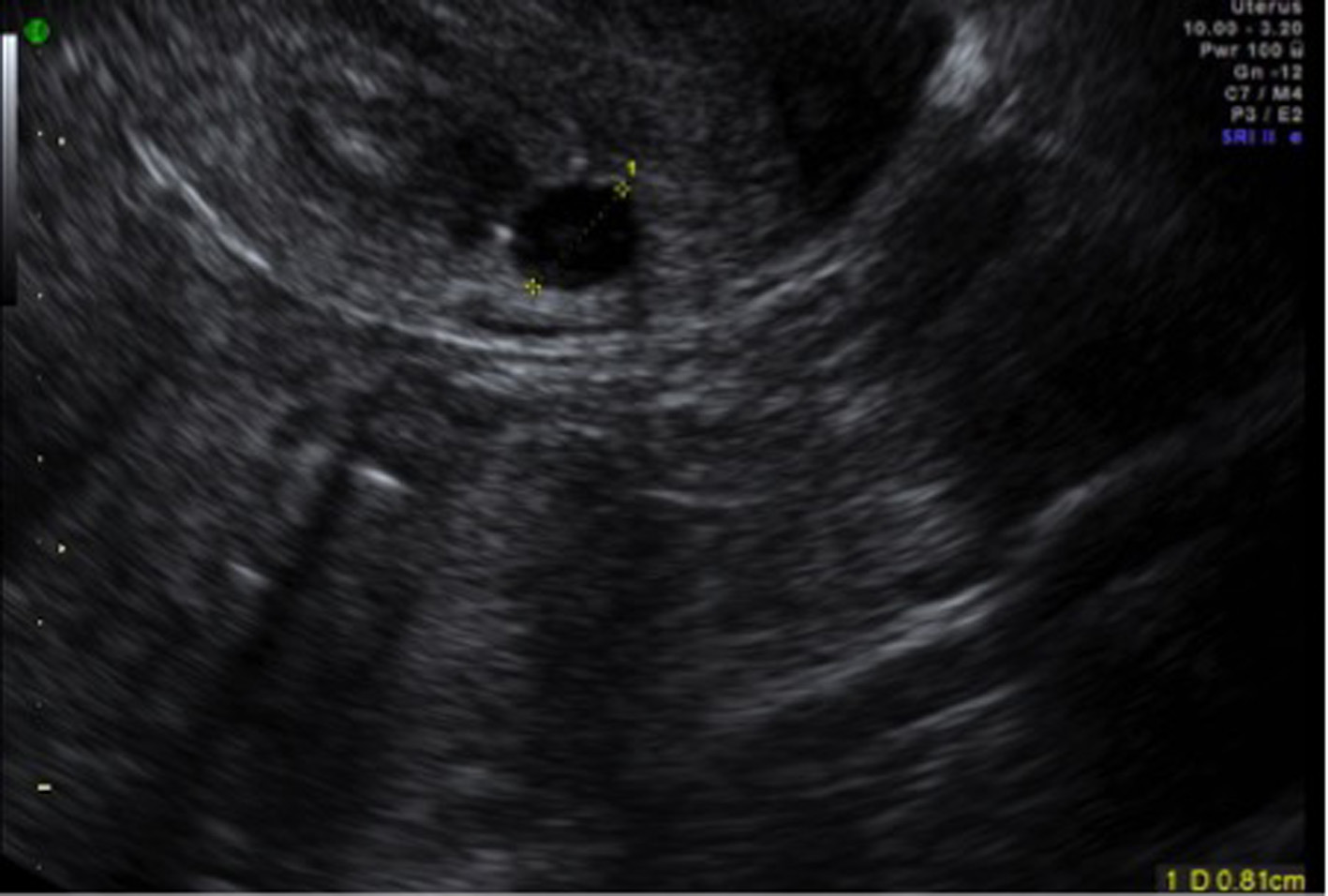 Click for large image | Figure 4. Gestational sac in cervix with a mixed echoic area above the sac. |
 Click for large image | Figure 5. Partial resolution of gestational sac with persistent adjacent mixed echoic area 6 weeks after methotrexate. |
| Discussion | ▴Top |
Spontaneous heterotopic pregnancy is extremely rare, although the incidence of heterotopic pregnancies can be up to 1% after artificial conception [1]. Spontaneous heterotopic cervical pregnancy is a much more rarer occurrence. Symptoms of cervical ectopic are similar to miscarriage and delayed diagnosis increases morbidity due to risk of major hemorrhage and hysterectomy. Ultrasound diagnosis is challenging. Ultrasound criteria described are cervical ballooning causing hour glass uterus [2], and presence of pregnancy tissue in cervix with closed internal os [3]. Negative sliding organ sign where the gestational sac in the cervix does not slide on applying gentle pressure with the probe and Doppler showing increased peri-trophoblastic blood flow around the pregnancy might be useful to differentiate cervical ectopic from products of conception in transit through cervix during miscarriage [4].
Several treatment options have been reported for cervical pregnancies including both medical and surgical management. Local or intramuscular methotrexate is an effective, fertility-preserving treatment option [5] when salvage of associated intrauterine pregnancy is not needed. In cervical ectopic, serum BHCG > 10,000 units and fetal heart beat are predictive factors for unsuccessful primary methotrexate treatment while factors such as age, parity, size of ectopic or presence of free fluid have no influence on outcome [6]. When fetal heart beat is present, methotrexate coupled with feticide increases the chance of success [7]. Following methotrexate, sonographic resolution of pregnancy takes longer than the BHCG normalization [8].
When conservation of associated intrauterine pregnancy is needed, surgical approaches such as ultrasound-guided aspiration of cervical pregnancy, removal of cervical pregnancy with ovum forceps, ultrasound-guided curetting with tamponade with Foley’s balloon or cervical stitch, hysteroscopic resection of cervical pregnancy, local injection of potassium chloride or hyperosmolar glucose with or without further surgical intervention have been reported [9, 10].
Reflection on good medical practice
This case has also highlighted some important good medical practices in the management of some common early pregnancy problems. 1) To monitor BHCG levels when scan finding is suggestive of complete/incomplete miscarriage without supporting clear evidence of passing products of conception. This lady initially presented with symptoms of potential miscarriage and the ultrasound was suggestive of possible minimal amount of retained products of conception. BHCG levels were followed up as there was no evidence of direct visualization of passing products of conception. It is good practice to follow BHCG levels especially when ultrasound is suggestive of complete miscarriage in the absence of clinical signs and symptoms. 2) When following up these patients, it is essential to monitor BHCG levels till < 20 or till urine pregnancy test is negative. When this patient had negative laparoscopy, BHCG levels were monitored after D&C. It is not only initial post-procedural drop in BHCG levels but further trend of fall should be also monitored [11, 12]. We could have missed the diagnosis if the patient was discharged after the initial drop in BHCG levels following D&C. It is good practice to monitor BHCG levels until < 20 [13], to confirm resolution of pregnancy or until urine pregnancy test is negative. In our case although there was an initial drop post procedure, there was a secondary rise. 3) While scanning, routine surveillance of cervix, cesarean scar, and cornual end of uterus should be done to avoid missing non-tubal ectopic pregnancy. In our case the secondary rise of BHCG after negative laparoscopy and D&C may be due to the following reasons: a) an early heterotopic tubal ectopic pregnancy too small to be visualized during laparoscopy; b) persistent trophoblastic activity due to molar pregnancy; c) ectopic pregnancy in unusual locations such as cervix, cesarean scar and cornual pregnancy missed during initial scan. In our case as the histology was negative for molar pregnancy, we performed a careful secondary surveillance scan to look at all the possible heterotopic ectopic sites which enables us to diagnose cervical pregnancy. Routine examination of cervix, cesarean scar, and interstitial portion of uterus is essential to avoid missing ectopic pregnancies in these unusual sites.
| References | ▴Top |
- Molloy D, Deambrosis W, Keeping D, Hynes J, Harrison K, Hennessey J. Multiple-sited (heterotopic) pregnancy after in vitro fertilization and gamete intrafallopian transfer. Fertil Steril. 1990;53(6):1068-1071.
pubmed - Hofmann HM, Urdl W, Hofler H, Honigl W, Tamussino K. Cervical pregnancy: case reports and current concepts in diagnosis and treatment. Arch Gynecol Obstet. 1987;241(1):63-69.
doi pubmed - Timor-Tritsch IE, Monteagudo A, Mandeville EO, Peisner DB, Anaya GP, Pirrone EC. Successful management of viable cervical pregnancy by local injection of methotrexate guided by transvaginal ultrasonography. Am J Obstet Gynecol. 1994;170(3):737-739.
doi - Jurkovic D, Hacket E, Campbell S. Diagnosis and treatment of early cervical pregnancy: a review and a report of two cases treated conservatively. Ultrasound Obstet Gynecol. 1996;8(6):373-380.
doi pubmed - Oyer R, Tarakjian D, Lev-Toaff A, Friedman A, Chatwani A. Treatment of cervical pregnancy with methotrexate. Obstet Gynecol. 1988;71(3 Pt 2):469-471.
pubmed - Bai SW, Lee JS, Park JH, Kim JY, Jung KA, Kim SK, Park KH. Failed methotrexate treatment of cervical pregnancy. Predictive factors. J Reprod Med. 2002;47(6):483-488.
doi - Hung TH, Shau WY, Hsieh TT, Hsu JJ, Soong YK, Jeng CJ. Prognostic factors for an unsatisfactory primary methotrexate treatment of cervical pregnancy: a quantitative review. Hum Reprod. 1998;13(9):2636-2642.
doi pubmed - Song MJ, Moon MH, Kim JA, Kim TJ. Serial transvaginal sonographic findings of cervical ectopic pregnancy treated with high-dose methotrexate. J Ultrasound Med. 2009;28(1):55-61.
pubmed - Kim JW, Park HM, Lee WS, Yoon TK. What is the best treatment of heterotopic cervical pregnancies for a successful pregnancy outcome? Clin Exp Reprod Med. 2012;39(4):187-192.
doi pubmed - Suzuki M, Itakura A, Fukui R, Kikkawa F. Successful treatment of a heterotopic cervical pregnancy and twin gestation by sonographically guided instillation of hyperosmolar glucose. Acta Obstet Gynecol Scand. 2007;86(3):381-383.
doi pubmed - Billieux MH, Petignat P, Anguenot JL, Campana A, Bischof P. Early and late half-life of human chorionic gonadotropin as a predictor of persistent trophoblast after laparoscopic conservative surgery for tubal pregnancy. Acta Obstet Gynecol Scand. 2003;82(6):550-555.
doi pubmed - Dumesic DA, Hafez GR. Delayed hemorrhage of a persistent ectopic pregnancy following laparoscopic salpingostomy and methotrexate therapy. Obstet Gynecol. 1991;78(5 Pt 2):960-962.
pubmed - RCOG green top guideline 21, management of tubal pregnancy.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
