| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website http://www.jcgo.org |
Case Report
Volume 5, Number 2, June 2016, pages 68-70
Recurrent Acute Appendicitis During the First Stage of Labor
Yoshinori Moriyamaa, Tomomi Kotania, c, Hiroyuki Tsudaa, Kazuhiro Ezakab, Chie Tanakab, Fumitaka Kikkawaa
aDepartment of Obstetrics and Gynecology, Nagoya University Graduate School of Medicine, Japan
bDepartment of Gastroenterological Surgery (Surgery II), Nagoya University Graduate School of Medicine, Japan
cCorresponding Author: Tomomi Kotani, 65 Tsurumai-cho, Showa-ku, Nagoya, Aichi 4668550, Japan
Manuscript accepted for publication March 29, 2016
Short title: Recurrent Appendicitis During Labor
doi: http://dx.doi.org/10.14740/jcgo397w
| Abstract | ▴Top |
A 32-year-old nulliparous Japanese woman presented with acute appendicitis at 12 weeks of gestation, which was successfully treated non-surgically with intravenous antibiotics. However, she had a relapse of acute appendicitis at 40 + 3 weeks of gestation and underwent emergent simultaneous cesarean section and appendectomy. Careful attention should be paid to the relapse of appendicitis after its successful conservative management.
Keywords: Acute appendicitis; Relapse; Labor onset; Conservative management; Chorioamnionitis
| Introduction | ▴Top |
Acute appendicitis is one of the most common abdominal emergencies, and it can also occur during pregnancy. When the symptoms are atypical, the prompt diagnosis of appendicitis is difficult. However, if the diagnosis is delayed, appendix perforation and peritonitis might develop, which lead to poor prognosis for both the mother and the baby. Prompt and accurate diagnosis and treatment are important in pregnant women with acute appendicitis. To our knowledge, this is the first detailed report on the clinical course of recurrent acute appendicitis that was diagnosed after the onset of labor.
| Case Report | ▴Top |
A 32-year-old nulliparous Japanese woman had acute appendicitis at 12 weeks of gestation and was conservatively treated with intravenous antibiotics at a hospital. She was referred to our hospital at 18 weeks of gestation for the management of gestational diabetes mellitus. Her pregnancy was managed with the cooperation of the internal medicine team at our hospital. Self-monitoring of blood glucose levels was started and resulted in good control, with a maximum postprandial blood glucose level of approximately 150 mg/dL. Blood glucose levels were controlled by diet alone, and medications, such as insulin, were not needed. At 40 + 3 weeks of gestation, she presented with right lateral abdominal pain and mild fever at 37.7 °C. The pain was ambiguous that it was very similar to the symptoms of the onset of labor. The cardiotocogram revealed a reassuring fetal status with a fetal heartbeat of 140 beats/min, moderate variability, and no deceleration and regular uterine contractions approximately 8 min apart, consistent with the first stage of labor. The patient was nauseous before the onset of abdominal pain, and the nausea could have been caused by labor or a manifestation of appendicitis. The gastroenterology surgical team was consulted because of the suspicion of recurrence of appendicitis. Transabdominal ultrasonography, a common diagnostic tool for appendicitis, was performed. However, the ultrasonogram was poor because of the presence of the fully enlarged uterus, and there were no findings suggestive of appendicitis or any other abnormality. The cervix was open at only 4 cm, and the amniotic membrane had not ruptured. Her blood test revealed a slightly elevated white blood cell count of 13.7 × 103/μL (neutrophils 11.8 × 103/μL), and it was unclear whether this was due to appendicitis. However, the serum C-reactive protein level increased to 7.09 mg/dL, and this led us to diagnose the recurrence of appendicitis. Computed tomography (CT) imaging is useful for both diagnosis and decision making for appendicitis because it provides information on the size and location of the appendix in cases that are difficult to diagnose by ultrasonography. However, CT was not performed due to concerns over its possible adverse effects on the fetus. The patient’s pain became severe; however, the progress of labor was slow. Therefore, we decided to perform emergent and simultaneous cesarean section and appendectomy to prevent perforation of the appendix and to protect the fetus from the adverse effects of maternal inflammation. During surgery, her appendix was found to be moderately swollen. A male baby was delivered, weighing 3,290 g with Apgar scores of 8 and 9 at 1 and 5 min after birth, respectively. The pH of the umbilical arterial blood gas was 7.298. The baby did not require intervention by neonatologists. However, meconium staining of the amniotic fluid was found during the operation. A pathological examination revealed that the patient had Blanc III chorioamnionitis (Fig. 1) and acute gangrenous appendicitis. The patient’s and the baby’s postoperative courses were uneventful, and they were discharged on the seventh day after the surgery.
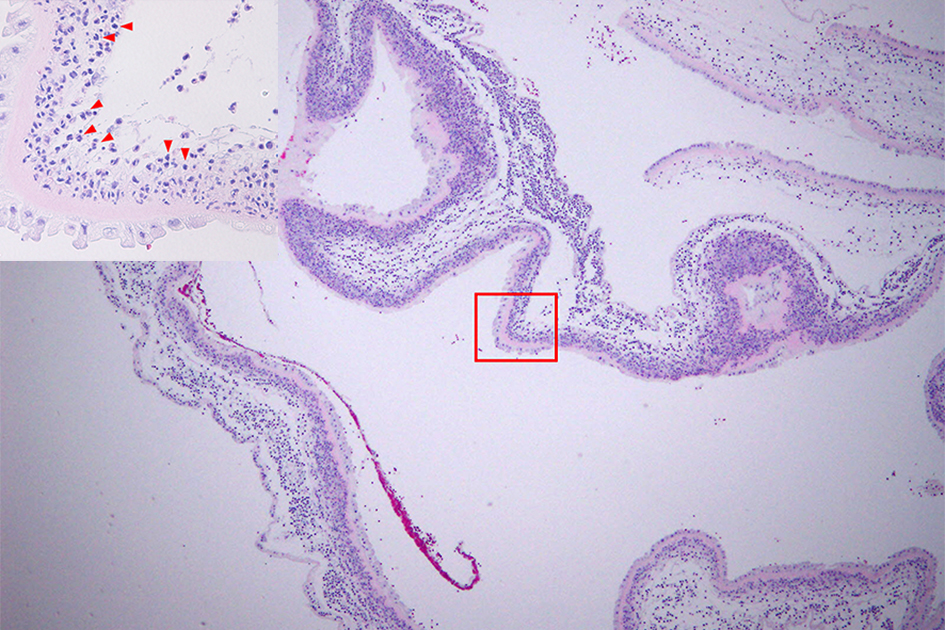 Click for large image | Figure 1. Hematoxylin-eosin staining of the placenta. The arrowheads indicate inflated neutrophils into the amnion, which is consistent with Blanc III chorioamnionitis. The original magnification is × 40 and that of the inset is × 400. |
| Discussion | ▴Top |
This case highlights several clinically important issues. At term pregnancy, the diagnosis of appendicitis is very difficult. In such instances, labor often starts concurrently. Appendicitis after 24 weeks of gestation is known to be accompanied by painful uterine contractions [1]. Symptoms of appendicitis are almost similar to those of labor and include lower abdominal pain, nausea, vomiting, anorexia, and mild fever. In addition, during pregnancy, manifestations of acute appendicitis can be mild in spite of its severity or can masquerade as uterine contractions induced by appendicitis. Therefore, it is very difficult to accurately and promptly diagnose appendicitis. Moreover, irrespective of the imaging modality, visualization of the appendix decreases with an advanced gestational period [2]. Other abdominal emergencies are sometimes challenging for the same reasons; however, recent reports have demonstrated that magnetic resonance imaging (MRI) is useful and reproducible in the diagnosis of suspected acute appendicitis during pregnancy [3, 4]. MRI is applicable in pregnant women, whereas CT imaging remains a concern because of irradiation of the fetus. This patient was able to be clinically diagnosed; however, one report revealed that the clinical diagnosis of acute appendicitis has been proven to be wrong in 93% of patients [3]. Unnecessary surgical intervention should also be avoided.
Clinicians should also be mindful of the relapse of appendicitis during pregnancy if it has been conservatively treated during early pregnancy. In our patient, gestational diabetes mellitus might have contributed to its relapse; however, pregnancy itself is a well-known risk factor for opportunistic infections and their progression. It might be better to perform appendectomy in early pregnancy appendicitis to avoid its relapse and the resulting complications. A population-based study showed that pregnant women with acute appendicitis have higher rates of adverse outcomes than non-pregnant women and that conservative management should be avoided [5]. The other study has reported that pregnant women with appendicitis are more likely to deliver preterm [6]. Further research is required for the management of acute appendicitis during pregnancy.
A previous study reported that the rate of fetal mortality rate was 8% and that mortality occurred in patients with perforated appendicitis [7]. Perforated appendicitis also significantly increases maternal morbidity rates [7]. Therefore, prompt treatment is thought to be important for preventing perforation. Moreover, our patient had a complication of progressive chorioamnionitis Blanc III. This was speculated to be the result of spreading inflammation from the appendix to the uterus. There are case reports on appendicitis complicated with chorioamnionitis [8-10], which is a well-known risk for neonatal complications. Therefore, prompt treatment might also prevent chorioamnionitis. Forced delivery should also be considered to protect the baby from a deteriorating intrauterine environment due to chorioamnionitis.
Acute appendicitis during pregnancy is difficult to diagnose; however, prompt treatment is required. In patients with conservative management, the risk of relapse during pregnancy should be kept in mind.
| References | ▴Top |
- Mourad J, Elliott JP, Erickson L, Lisboa L. Appendicitis in pregnancy: new information that contradicts long-held clinical beliefs. Am J Obstet Gynecol. 2000;182(5):1027-1029.
doi pubmed - Debnath J, Sharma P, Maurya V. Diagnosing appendicitis during pregnancy: which study when? Am J Obstet Gynecol. 2016;214(1):135-136.
doi pubmed - Burke LM, Bashir MR, Miller FH, Siegelman ES, Brown M, Alobaidy M, Jaffe TA, et al. Magnetic resonance imaging of acute appendicitis in pregnancy: a 5-year multiinstitutional study. Am J Obstet Gynecol. 2015;213(5):693 e691-696.
- Ditkofsky NG, Singh A. Challenges in magnetic resonance imaging for suspected acute appendicitis in pregnant patients. Curr Probl Diagn Radiol. 2015;44(4):297-302.
doi pubmed - Abbasi N, Patenaude V, Abenhaim HA. Management and outcomes of acute appendicitis in pregnancy-population-based study of over 7000 cases. BJOG. 2014;121(12):1509-1514.
doi pubmed - Abbasi N, Patenaude V, Abenhaim HA. Evaluation of obstetrical and fetal outcomes in pregnancies complicated by acute appendicitis. Arch Gynecol Obstet. 2014;290(4):661-667.
doi pubmed - Yilmaz HG, Akgun Y, Bac B, Celik Y. Acute appendicitis in pregnancy - risk factors associated with principal outcomes: a case control study. Int J Surg. 2007;5(3):192-197.
doi pubmed - Bard JL, O'Leary JA. Chorioamnionitis and appendiceal abscess. A case report. J Reprod Med. 1994;39(4):321-323.
pubmed - Belli S, Yalcinkaya C, Ezer A, Bolat F, Colakoglu T, Simsek E. Stump appendicitis and chorioamnionitis due to incomplete appendectomy: a case report. Turk J Gastroenterol. 2011;22(5):540-543.
doi pubmed - Managoli S, Chaturvedi P, Vilhekar KY, Gupta D, Ghosh S. Perforated acute appendicitis in a term neonate. Indian J Pediatr. 2004;71(4):357-358.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
