| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website http://www.jcgo.org |
Case Report
Volume 7, Number 1, March 2018, pages 23-25
Ogilvie’s Syndrome With Cecal Perforation Post Cesarean Section: A Case Report
Dennis Wei Jian Gonga, b, Victor Jian Yuan China
aDepartment of Obstetrics & Gynaecology, NorthWest Regional Hospital, University of Tasmania (UTAS), Australia
bCorresponding Author: Dennis Wei Jian Gong, Department of Obstetrics & Gynaecology, Royal Women’s Hospital, Melbourne, Australia
Manuscript submitted January 10, 2018, accepted March 8, 2018
Short title: Ogilvie’s Syndrome With Cecal Perforation
doi: https://doi.org/10.14740/jcgo474w
| Abstract | ▴Top |
This case report seeks to highlight a rather uncommon yet important complication of cesarean section (CS) Ogilvie’s syndrome (OS). This syndrome describes the phenomenon of an acute colonic pseudo-obstruction (ACPO), often without an obvious mechanical cause. The obstruction can then lead to bowel perforation or ischemia. We present a case of a young, healthy primigravida who developed OS on day 6 post CS, complicated by a perforated cecum and fecal peritonitis. We will summarize the sequence of events, management and outcome of the patient in this report. We hope that this report will help guide obstetricians and midwifery staff to promptly recognize and treat complications of OS.
Keywords: Ogilvie’s syndrome; Cesarean section; Cecal perforation
| Introduction | ▴Top |
In 1948, Sir William H. Ogilvie first coined the term Ogilvie’s syndrome (OS) following his observation on two of his patients with metastatic cancer [1]. He describes the clinical scenario of acute massive dilatation of colon with no mechanical obstruction of the distal colon.
OS still remained as an under-recognized condition. Its true incidence is still a mystery, partly due to the nature of the mild cases which tend to resolve spontaneously. Furthermore, there are no reliable national or international data to suggest its frequency [2]. However, delay in diagnosing has a significant direct correlation with mortality rates. It has been suggested that there is a 15% mortality rate in a healthy patient who received early intervention with no complications compared to 36-50% mortality rate in someone with a perforation or ischemic bowel [3].
OS does not have any age predilection although it was observed more often in the elderly patients as well as those with multiple co-morbidities. It has a male/female ratio of 1.5:1 [4]. In the obstetrics setting, cesarean section (CS) was noted to be the most common procedure associated with OS, even though, it has also been reported to occur following vaginal birth and forceps assisted delivery [4-6]. The UK Confidential Enquiry into Maternal and Child Health (CEMACH) 2000 - 2002 report mentioned four deaths from OS, all following CS [7].
However, despite a rising rate of CS occurring worldwide, OS remains a relatively rare condition that deserved prompt recognition. Clinically, it would be rather challenging to differentiate between OS and paralytic ileus in the initial stage.
| Case Report | ▴Top |
A 19-year-old G1P0 presented for induction of labor (IOL) as she was post-date at 41 weeks. Antenatal care had been uneventful, and she was categorized as a low-risk pregnancy. She was induced with 1 mg of prostaglandin gel followed by artificial rupture of membrane (ARM) the subsequent day, which showed the presence of light meconium stained liquor. Her labor was augmented with oxytocin and routine labor monitoring was commenced with no abnormal recordings throughout labor. Following 12 h of active labor with good progress initially, it then arrested at 8 cm. On examination, the cervix was found to be 8 cm dilated and baby was in direct occiput-posterior position. Subsequently, a category 2 emergency CS for failure to progress was initiated.
CS went smoothly, and abdomen entered via Joel Cohen technique. The peritoneal cavity and pelvic organs appeared normal. No electro-coagulation instruments were used during the procedure. Baby was delivered via Wrigley’s forceps, weighing 4.6 kg. The Apgar score was 9 at 1 min and 9 at 5 min. The estimated blood loss was 500 mL. No bowel or bladder injury was observed intra-operatively.
Post-operatively, her recovery was slow due to pain and not passing flatus. There was documented bowel sound and distended abdomen on day 3. However, due to the fact that she opened her bowel on post-operative day 3, no further investigations were carried out. She then requested to be discharged home on day 4 post-operatively feeling well.
She presented to the emergency department on day 6 post-operatively with recurrent vomiting, generalized abdominal pain and distension. She also mentioned that she did open her bowel but it was different from her normal routine and her abdomen was so distended that she felt “she is pregnant again at 40 weeks”. Apart from these symptoms, she had been breast feeding and bonding well with baby.
Clinically, she was afebrile; however, she was having tachycardia and generalized tenderness elicited all over her abdomen. She also specifically mentioned bilateral shoulder tip pain. Her blood results came back with markedly elevated CRP of 612 and white cell count of 12.1 × 109/L. On imaging, abdominal X-ray showed distended loop of small and large bowel with positive Rigler’s sign, suggestive of perforation (Fig. 1). This was confirmed on CT scan, which showed a large perforation, presumably in the cecal region (Fig. 2).
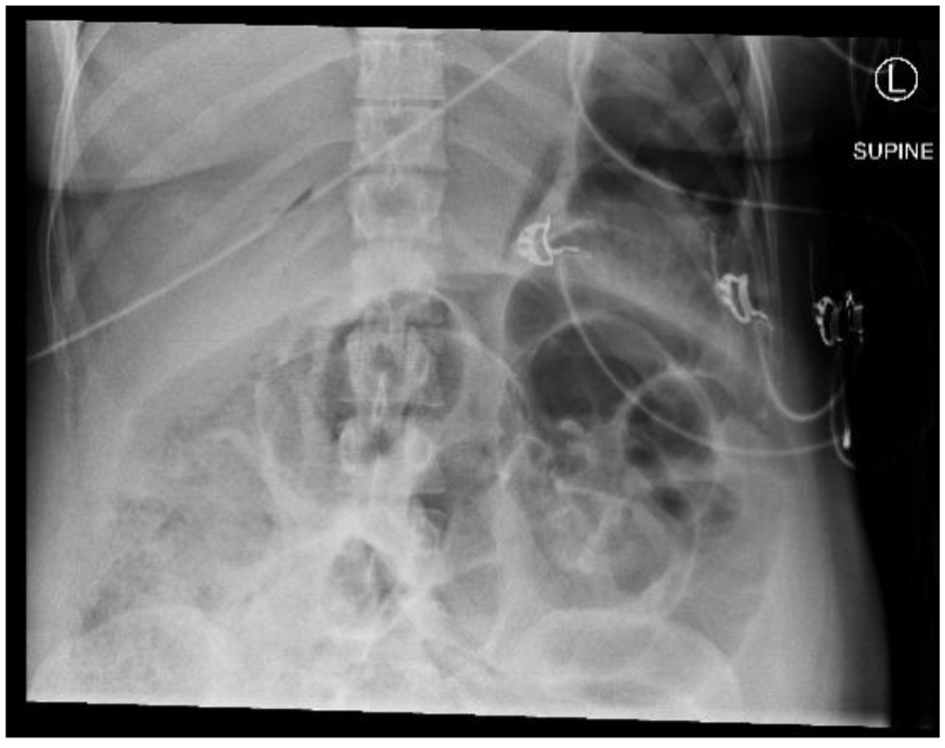 Click for large image | Figure 1. Diffuse gas distended loops of small and large bowel with some fecal loading noted in the cecum and right hemicolon. Suspicion of free gas with positive Rigler sign. |
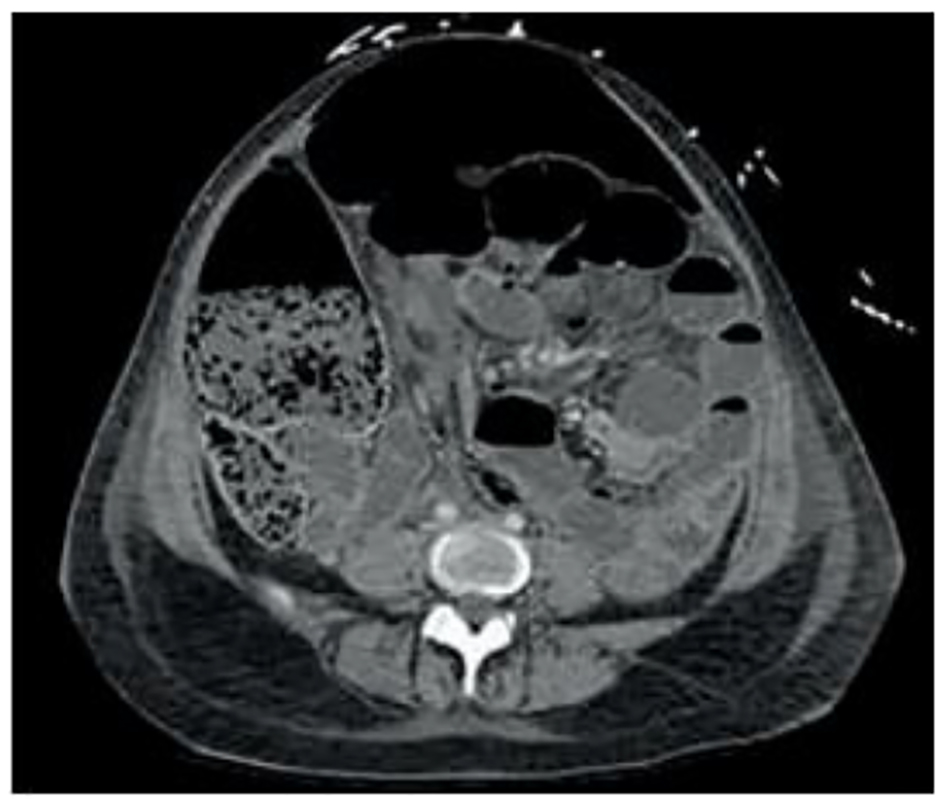 Click for large image | Figure 2. Large perforation with complex fluid and fecal material centered in the right lower quadrant favoring cecal pole source. |
She was brought to the theater for an emergency laparotomy. It was a joined operation by both the obstetric and general surgical team. The peritoneum was filled with fecal material and a perforation was seen at the cecum measuring approximately 5 cm in diameter. Approximately 5 L of fecal-purulent fluid was drained. A right hemi-colectomy was performed with end ileostomy and VAC dressing was applied. Following the primary laparotomy, she subsequently underwent three more exploratory laparotomies due to multiple collections, wound dehiscence and abdominal cavity washout.
Her recovery post-operatively was complicated by persistent sepsis requiring extensive antibiotics and inotropic support, prolonged intubation, multiple re-laparotomy, bilateral pleural effusions and pulmonary embolism.
The patient in our case was finally discharged home 35 days post primary laparotomy with an ileostomy. She is to remain on oral antibiotics for the next 4 weeks and rivaroxaban for 3 months (treatment for pulmonary embolism).
| Discussion | ▴Top |
The hallmark symptom of OS is marked abdominal distension developing over a short time frame [2]. Often this is associated with abdominal pain, nausea and vomiting. The woman is typically 2 - 12 days post CS [4]. As mentioned earlier, the signs and symptoms may initially mimic paralytic ileus. However, in OS, bowel sounds are often reported to be higher pitched and hyperactive [8]. In addition, the patient may still be able to pass small amount of fecal fluid and flatus. Abdominal pain in OS usually manifests as dull crampy sensation with no specific localization, typical of hollow viscus distension. This may then progress to localize over the right iliac fossa, indicating impending rupture of the cecum [9].
Patient is usually tachycardic, afebrile (pyrexia might indicate sepsis) and may be hypotensive. Laboratory results might not be very helpful in the first instance. In the acute setting, a plain erect abdominal X-ray would be most helpful in terms of narrowing down the list of differential diagnosis. This may show a typical picture of large bowel dilatation, especially the cecum with or without pneumoperitoneum. A CT of abdomen can then be requested to confirm the diagnosis of OS and more importantly to measure the cecal diameter, which would aid in the management and outcome of patient.
The exact etiology of OS is still poorly understood. However, the current consensus is that there is an imbalance of sympathetic and parasympathetic innervation of the colon [4]. Physiologically, the parasympathetic system increases the motility of the colon while the sympathetic system does the exact opposite. In a large analysis of 400 cases of OS, it was suggested that there is a temporary neuropraxia of the sacral parasympathetic outflow (S2-S4) [10]. This finding may help to explain OS post CS; however, this is yet to be confirmed.
The cecum, being the part of colon with the thinnest wall and largest diameter, makes it especially vulnerable to perforation. This can be explained by the Law of Laplace which states that the tension in the wall of a hollow viscus is directly proportional to its radius and intraluminal pressure [11].
Management of OS has been classically divided into conservative/medical and surgical. These options are dependent upon the cecal diameter, which in turn is dependent on early recognition of the condition. In general, cecal dilatation of less than 10 cm can be managed conservatively provided there are no signs of perforation [4]. This involves the patient being kept nil by mouth and use of nasogastric decompression. Any narcotic analgesics and anti-cholinergic drugs should be stopped.
Medical therapy involves the use of neostigmine, which promotes colon motility by inhibiting acetylcholinesterase. A small trial done in 1999 has shown that 50% of patients had immediate response (within 30 min, passing of flatus and reduced abdominal distension) and 73% had a sustained response (lasted over 3 h, of reduced cecal diameter) [12]. Neostigmine is given intravenously, 2.5 mg over 3 - 5 min. Colonoscopic decompression can be used next if treatment with neostigmine failed. This however has a variable success rate (61-78%) with a recurrence rate of 40% [13, 14].
Any signs of bowel perforation would warrant a surgical management. This usually entails laparotomy with bowel resection and formation of a stoma.
Conclusion
We hoped that this case on OS has managed to once again highlight the importance of this rare yet sinister condition, especially to our obstetric colleagues. It is important to maintain a high index of suspicion in the post CS patient presenting with progressive abdominal distension, despite the presence of falsely reassuring bowel sounds and passage of flatus. It cannot be stressed enough the importance of early diagnosis and intervention in preventing a catastrophic outcome to an otherwise young, healthy lady in her reproductive years.
Conflict of Interest
No conflict of interest arises from this case as the authors were not sponsored by any organization.
Author Contributions
Dr. Chin is the O&G Registrar involved in the cesarean section of the patient while Dr. Gong is the O&G Resident admitting the patient during presentation to the emergency department as well as participating in the joined laparotomy. They are both active participants in the post-operative care of the patient and Dr. Gong is the first author in the final write-up.
| References | ▴Top |
- Ogilvie H. Large-intestine colic due to sympathetic deprivation; a new clinical syndrome. Br Med J. 1948;2(4579):671-673.
doi pubmed - Carpenter S, Holmstorm B. Ogilvie Syndrome. www.eMedicine.com/med/topic2699.htm
- Norton-Old KJ, Yuen N, Umstad MP. An obstetric perspective on functional bowel obstruction after caesarean section: a case series. J Clin Gynecol Obstet. 2016;5(1):53-57.
doi - Kakarla A, Posnett H, Jain A, George M, Ash A. Review acute colonic pseudo-obstruction after caesarean section. The Obstetrician & Gynaecologist. 2006;8:207-213.
doi - Nanni G, Garbini A, Luchetti P, Nanni G, Ronconi P, Castagneto M. Ogilvie’s syndrome (acute colonic pseudo-obstruction): review of the literature (October 1948 to March 1980) and report of four additional cases. Dis Colon Rectum. 1982;25(2):157-166.
doi pubmed - Kakarla A, Posnett H, Jain A, Ash A. Acute pseudo-obstruction of the colon (Ogilvie’s syndrome) following instrumental vaginal delivery. Int J Clin Pract. 2006;60(10):1303-1305.
doi pubmed - Lewis G, Drife J. editors. Why mothers die 2000-2002. Condifential enquiry into maternal and child health. London: RCOG Press; 2004. p. 232-233.
- Laskin MD, Tessler K, Kives S. Cecal perforation due to paralytic ileus following primary caesarean section. J Obstet Gynaecol Can. 2009;31(2):167-171.
doi - Munro A. Large bowel obstruction. In: Wills BW. Paterson-Brown S, editors. Hamilton Bailey’s emergency surgery. 13th ed. London: Hodder Arnold; 2000. p. 436-439.
- Vanek VW, Al-Salti M. Acute pseudo-obstruction of the colon (Ogilvie’s syndrome). An analysis of 400 cases. Dis Colon Rectum. 1986;29(3):203-210.
doi pubmed - Brock W. Volvulus of the cecum. West J Surg Obstet Gynecol. 1954;62(1):12-17.
pubmed - Ponec RJ, Saunders MD, Kimmey MB. Neostigmine for the treatment of acute colonic pseudo-obstruction. N Engl J Med. 1999;341(3):137-141.
doi pubmed - Eisen GM, Baron TH, Dominitz JA, Faigel DO, Goldstein JL, Johanson JF, Mallery JS, et al. Acute colonic pseudo-obstruction. Gastrointest Endosc. 2002;56(6):789-792.
doi - Rex DK. Colonoscopy and acute colonic pseudo-obstruction. Gastrointest Endosc Clin N Am. 1997;7(3):499-508.
pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
