| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website http://www.jcgo.org |
Original Article
Volume 8, Number 1, March 2019, pages 1-8
Timing of an Elective Repeat Cesarean Delivery at Term: Addressing the Controversy
Mohamad K. Ramadana, Ahmad Abdulrahima, Saad Eddine Itania, Mohamad Houranib, Fadi G. Mirzac, d, e
aDepartment of Obstetrics and Gynecology, Division of Maternal Fetal Medicine, Makassed General Hospital, Beirut, Lebanon
bDepartment of Pediatrics, Makassed General Hospital, Beirut, Lebanon
cDepartment of Obstetrics and Gynecology, Division of Maternal Fetal Medicine, American University of Beirut Medical Center, Beirut, Lebanon
dDepartment of Obstetrics and Gynecology, Division of Maternal Fetal Medicine, Columbia University College of Physicians and Surgeons, New York, NY, USA
eCorresponding Author: Fadi G. Mirza, Department of Obstetrics and Gynecology, Division of Maternal Fetal Medicine, American University of Beirut Medical Center, Beirut 11-0236, Lebanon
Manuscript submitted November 15, 2018, accepted January 25, 2019
Short title: Timing of ERCD at Term
doi: https://doi.org/10.14740/jcgo526
| Abstract | ▴Top |
Background: Although most professional societies recommend scheduling elective repeat cesarean deliveries (ERCDs) at 39 weeks, some care providers have started to practice scheduling at earlier timing for various reasons. The objective of our study was to compare the outcomes of scheduling ERCDs at 3 different weeks at term.
Methods: In a prospective, observational cohort study conducted over a 2-year period, 339 parturients were scheduled for ERCD at 37, 38 or 39 weeks. In an intention-to-treat approach, we are reporting the rates of delivery before schedule, maternal and neonatal morbidity corresponding to each of these three decisions.
Results: A total of 5.3% of deliveries scheduled at 37 weeks were performed before schedule, compared to 16.1% and 46.7% of those scheduled at 38 and 39 weeks, respectively (P < 0.0001). Likewise, delivery outside working hours demonstrated a trend that increased with gestation but was only statistically significant between 38 versus 39 weeks. As expected, a significant improvement was identified for neonatal intensive care unit (NICU) admissions and respiratory morbidity between 37 versus 39 weeks but was minimal between 38 versus 39 weeks. There was no difference in maternal outcome parameters among the three categories.
Conclusions: Individualizing patients, according to their risk of spontaneous labor, added obstetric complications if progressed in pregnancy and maternity resources should be integrated in the decision of scheduling ERCD. Scheduling at 38 weeks might curb unplanned delivery rate at the expense of a marginal, though non-significant, increase of neonatal respiratory morbidity.
Keywords: Scheduling elective repeat cesarean delivery; Unplanned delivery; Weeks of gestation
| Introduction | ▴Top |
The American College of Obstetricians and Gynecologists (ACOG) and the American Academy of Pediatrics (AAP) have jointly issued clinical practice guidelines that strongly recommend deferring elective delivery until 39 completed weeks of gestation [1]. This recommendation has been primarily based on a significant body of evidence demonstrating improved neonatal respiratory outcome at 39 weeks compared to 37 weeks [2-4]. This approach, however, has been shown to increase the risk of macrosomia, meconium-aspiration syndrome and stillbirth [5-6]. In turn, the interplay between maternal outcome and gestational age at the time of delivery has been inconclusive with conflicting data [7-10]. It is noteworthy that a paradigm shift has recently emerged, as a result of several recent studies that suggested less favorable outcomes when a cesarean delivery was performed on an emergent basis before its scheduled time, such as in the event of ruptured membranes or labor prior to 39 weeks [11-15]. In spite of the fact that most societies still recommend deferring scheduling elective repeat cesarean deliveries (ERCDs) till 39 weeks, unless clinically indicated, some providers are actually practicing earlier timing of delivery such as at 37 or 38 weeks. The objective of our study was to examine, in a contemporary cohort, the rate of performing non-elective (unplanned) cesarean delivery prior to its scheduled time and to investigate whether scheduling ERCDs at 39 weeks yielded the best maternal and neonatal outcomes when compared with 37 and 38 weeks.
| Materials and Methods | ▴Top |
A prospective observational cohort study was conducted at Makassed General Hospital, a teaching tertiary care facility that provides services for approximately 1,200 deliveries per year in the setting of a level III neonatal intensive care unit (NICU). The study proposal was approved by the Institutional Review Board. Data were prospectively collected from the electronic medical records within 48 h of mother/newborn discharge. During the 2-year study period, a total of 2,183 were delivered at our facility with an overall cesarean rate of 43.5%. Of the cesarean deliveries performed, 43.8% were repeat deliveries. Scheduling of delivery was at the discretion of the primary provider as per his/her routine practice.
All parturients with a singleton gestation, with history of at least one previous low-transverse cesarean delivery, and with a plan for an ERCD at 37, 38 or 39 weeks were eligible for study recruitment. Exclusion criteria included preterm delivery, failed trial of labor after cesarean delivery (TOLAC), fetal demise, major fetal congenital malformations, polyhydramnios, previous myomectomy, congenital malformations, and cervical cerclage during the index pregnancy. Gestational age was determined on the basis of last menstrual period confirmed by an ultrasound done in the first half of pregnancy. Ninety-five percent of this cohort was private patients who started their regular antenatal visits early. Assignment to the gestational age category was achieved by rounding to the nearest complete week, such that the 37-week category included patients scheduled between 36 + 4/7 and 37 + 3/7 weeks; the 38-week category included those scheduled between 37 + 4/7 and 38+ 3/7 weeks; and the 39-week category included those scheduled between 38 + 4/7 and 39 + 3/7. A total of 339 subjects included in the study were distributed as follows: 38 cases in the 37-week category, 211 in the 38-week category, and 90 in the 39-week category (Fig. 1). Maternal co-morbidities were selected according to a previous publication by Bateman et al [16]. Obesity was defined as a current weight greater than 91 kg during pregnancy [17]. Labor was defined as having three or more painful and regular uterine contractions in a 10-min interval during a 60-min of tocodynamometer tracing. Three working shifts exist at our institution and are as follows: 7 am to 3 pm, 3 pm to 11 pm and 11 pm till 7 am. The latter two were considered as outside regular hours, while the night shift specifically reserved for deliveries between 11 pm and 7 am. Deliveries occurring on Saturdays and Sundays were considered weekend deliveries, as hospital policy prohibits scheduling elective cases on these days. All patients received prophylactic preoperative antibiotics and analgesics postpartum. Patients received thromboprophylaxis according to their risk assessment.
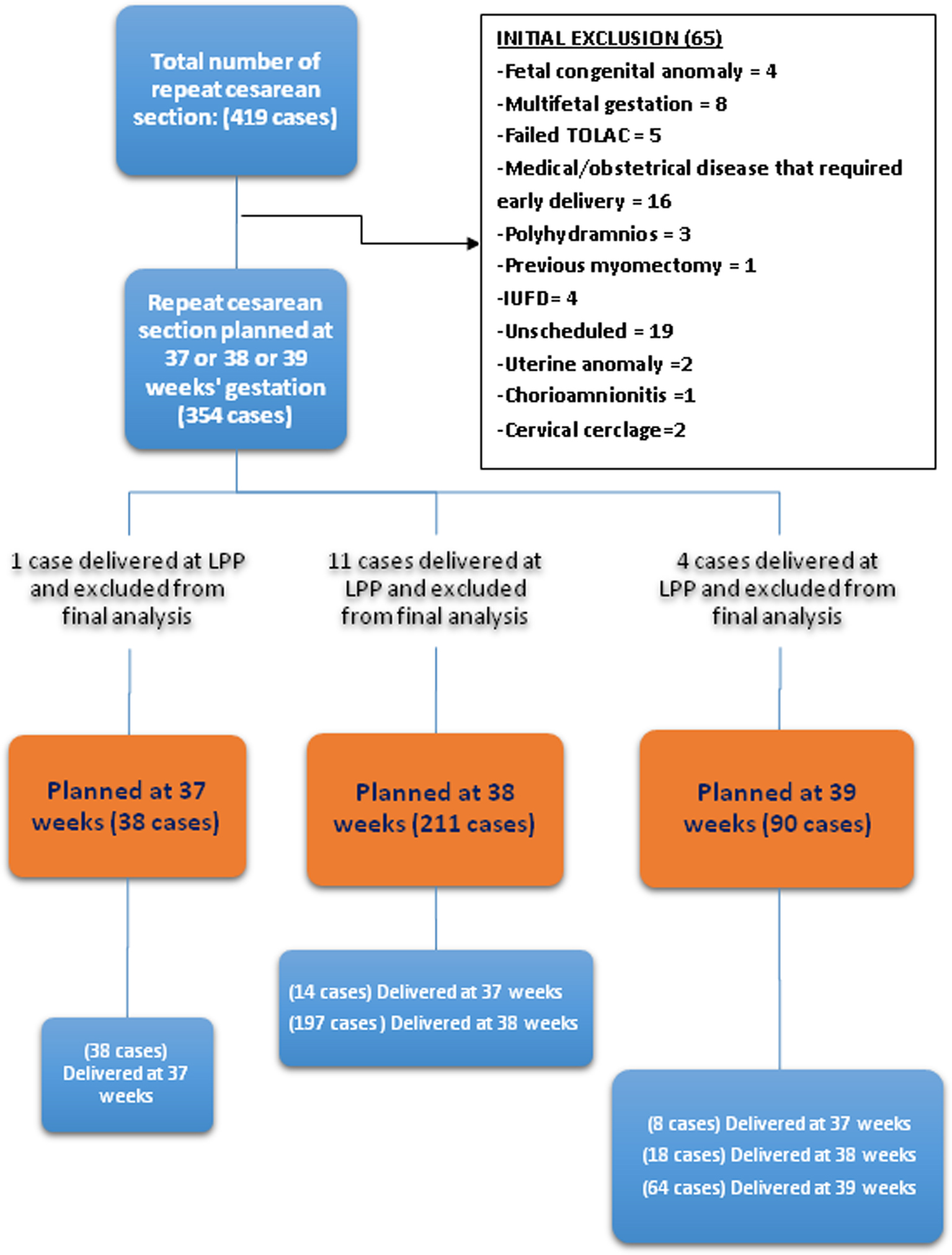 Click for large image | Figure 1. Study flow chart. |
Individual maternal outcome variables included the following: febrile illness was defined as temperature ≥ 38 °C taken orally and in whom no site of infection was identified and where subjects did not receive postpartum misoprostol. An adverse maternal outcome composite included the occurrence of any of the following: development of postpartum febrile illness, endomyometritis, need for blood transfusion, deep vein thrombosis/pulmonary embolism, organ injury, cesarean hysterectomy, postpartum hemorrhage and thinning or dehiscence of the previous cesarean scar. Thinning and dehiscence were subjectively determined by the delivering obstetricians and defined as a disruption of a part or the entire uterine muscle but with intact serosa. Wound infection was defined as superficial or deep infection involving the skin incision site. Endomyometritis was defined as persistent postpartum fever, with or without foul-smelling lochia, with or without abnormal uterine tenderness in the absence of clinical or laboratory findings suggesting other source of infection. The neonatal outcome variables collected were NICU admission rate due to any cause and NICU admission due to respiratory morbidity. Another composite outcome calculated was the development of any maternal or neonatal adverse outcome. Delivery logistics included operative time, need for general anesthesia and delivery on weekends or during night shift.
We intended to study a group of independent cases (scheduled at 39 weeks) and controls (scheduled at 37 and 38 weeks) with two controls per case. Prior data indicate that unplanned cesarean rate in experimental subjects was 0.41 (14); thus, we needed to study 67 experimental subjects and 134 controls to be able to reject the null hypothesis (that the unplanned, non-elective cesarean delivery rates for experimental and control subjects are equal) with β = 80 % and α = 5% and an expected relative risk (RR) of 0.5. Power and Sample (PS) calculations software version 3.1.2 was used to calculate sample size. Chi-square test was used to calculate the statistical difference of dichotomous variables between groups, whereas ANOVA was used for continuous variables. P value of less than 0.05 was considered statistically significant. A logistic regression model was constructed to determine the most significant factors predicting the rate of the primary outcome (non-elective cesarean sections). Statistical analysis was performed using IBM-SPSS (version 22).
| Results | ▴Top |
The rate of unplanned cesarean deliveries (the primary outcome) increased with advancing gestational age, and the difference was statistically significant between the three gestational age groups (P < 0.0001). Labor accounted for around 80% (n = 63/78) of unplanned cesarean deliveries, while the remaining 20% (n = 15/78) were attributed to the following obstetric conditions: premature rupture of membrane (PROM) (n = 8), fetal growth restriction/distress (n = 4), preeclampsia (n = 1), abruptio placenta (n = 1), and placenta previa (n = 1).
Another observation was that 73.4% of ERCD were scheduled before 39 weeks’ gestation (11.2% at 37 and 62.2% at 38 weeks) and this was probably influenced by a high rate of high-order cesareans in this cohort. Although this was an observational study where scheduling and management of patients were at the discretion of their caregivers and not according to an internal policy or study protocol, a trend in the scheduling process was observed among obstetricians who tended to schedule most cases of (≥ tertiary cesarean sections) around 37 to 38 weeks, while cases of secondary cesareans were scheduled at 39 weeks, which resulted in higher-order cesarean sections being scheduled at earlier gestational age (Fig. 2). This, in turn, caused more obese patients with higher mean parity and older age to be clustered in the 37 week group, which was statistically significant when compared to 38- and 39-week groups. Other demographic parameters were equally distributed among the three groups (Table 1).
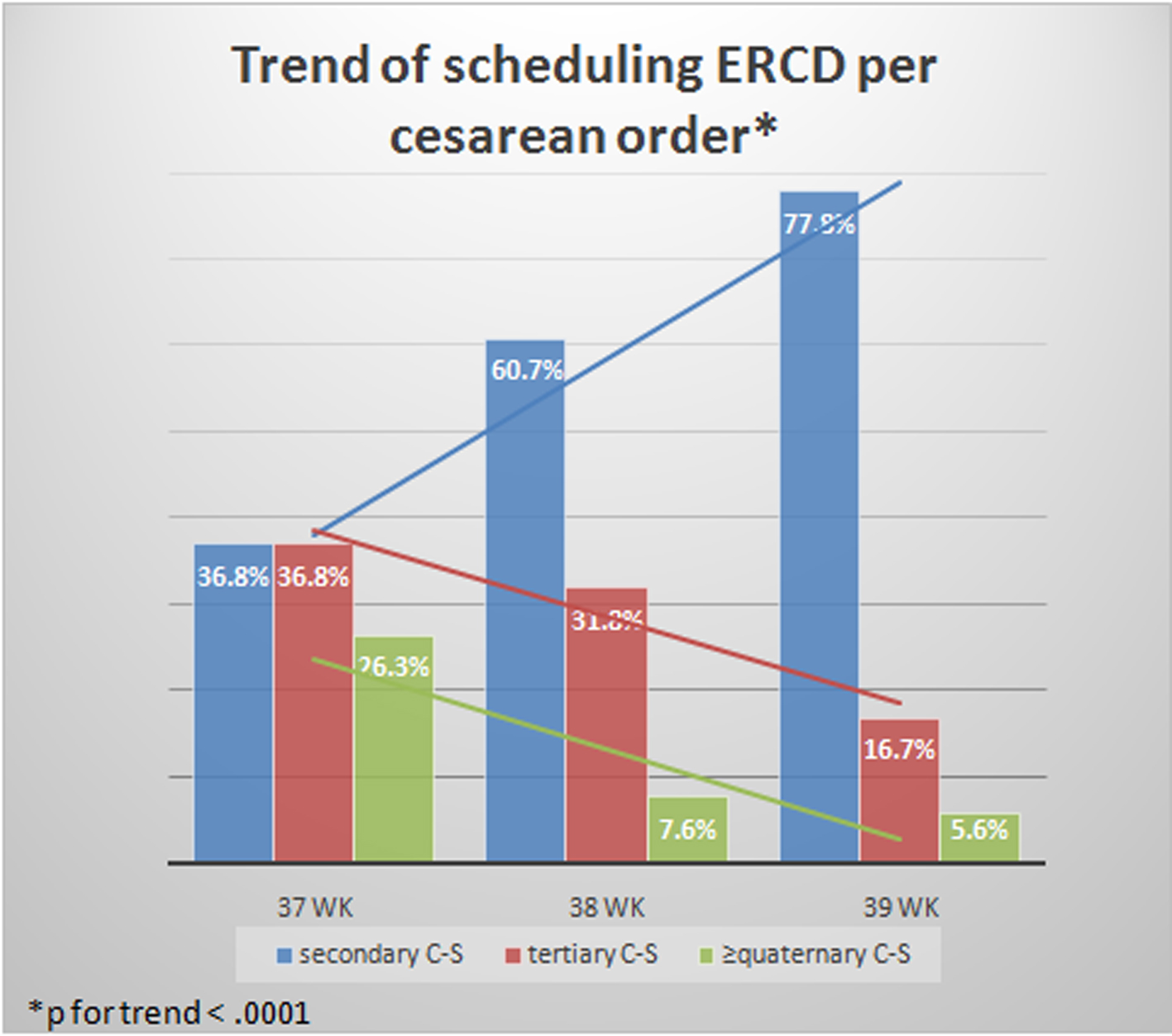 Click for large image | Figure 2. Tendency among local obstetricians for scheduling ERCD according to order of cesarean section. |
 Click to view | Table 1. Demographic Features of the Study Population |
Other delivery-related logistic parameters like delivery at weekend, outside regular working hours or during night shifts have similarly showed the same statistically significant trend that worsened with increasing gestation. Mean gestational age at delivery was also significantly different, as was the mean schedule-delivery interval in cases who presented in labor at each week. No difference was noted either in mean operative time or the rate of general anesthesia among groups (Table 2).
 Click to view | Table 2. Effect of Scheduling on Delivery Logistics |
None of maternal outcome parameters (maternal morbidity, febrile illness, thinning, dehiscence or thinning/dehiscence) showed statistically significant trend among the three categories. Likewise, the composite (any maternal morbidity/neonatal morbidity) was not different among the three groups. NICU admission due to respiratory morbidity or any cause, however, was statistically different among the groups: being worse at 37 week to ameliorate at 38 week and to show further improvement at 39 week (Table 3).
 Click to view | Table 3. Maternal and Neonatal Outcomes in Relation to Scheduled Week of Gestation |
The effect of transition from 37 to 38 and 39 weeks with respect to changes in RR was calculated. NICU admission rate and respiratory morbidity showed significant protective effect between 37 and 38 weeks but not between 38 and 39 weeks. However, delivery at weekend or during night shifts exhibited a negative effect between 38 and 39 weeks but not between 37 and 38 weeks (Table 4). A forward logistic regression model was constructed to study the influence of five variables on the rate of unplanned cesarean delivery and included mean maternal age, mean parity, obesity, age of scheduled delivery, and cesarean section order as predictors of unplanned delivery. The only significant factor that impacted the rate of unplanned cesarean delivery was scheduled time while the remaining variables did not manifest a significant role (Table 5).
 Click to view | Table 4. Relative Risk Changes According to Scheduled Week of Gestation |
 Click to view | Table 5. Multivariate Analysis of Risks for Primary Outcome |
| Discussion | ▴Top |
Our study demonstrated a number of important findings. As expected, scheduling a cesarean delivery at 39 weeks conferred the most favorable neonatal outcome. The improvement in neonatal outcomes with advancement of gestation was considerable between 37 and 38 weeks but less between 38 and 39 weeks in terms of the rate of NICU admissions and neonatal respiratory morbidity. Nonetheless, it was noted that nearly half cases scheduled at 39 weeks presented in labor and required delivery prior to their scheduled delivery. Of these, 41.1% of deliveries occurred outside working hours, 11.1% during weekends, and 8.9% during night shifts. The mean difference in time interval for those presented in labor before their scheduled time was 2.0 days ± 0.64 for those scheduled at 37 weeks, 5.9 days ± 2.0 and 8.7 days ± 4.8 for those scheduled at 38 and at 39 weeks respectively. It is noteworthy that scheduling delivery at 38 weeks’ gestation resulted in a 3-fold decline in the risk of unplanned cesarean deliveries with a non-significant increase in neonatal morbidities. In turn, scheduling delivery at 37 weeks’ gestation was accompanied with another three-fold decline in the rate of unplanned cesarean deliveries but resulted in a statistically significant worsening of neonatal outcomes.
The ACOG recommendation to delay scheduling ERCD until 39 completed weeks’ gestation was released following accumulation of evidence showing that the lowest rate of neonatal complications was encountered when delivery occurred at 39 weeks’ gestation. However, a significant proportion of obstetricians do not comply with these recommendations for a myriad of reasons. A study from the USA showed that scheduling an ERCD prior to 39 weeks of gestation occurred in around 50% of cases [4]. In our study, adherence to the guidelines was apparent only when scheduling elective secondary cesarean delivery, while scheduling higher order ERCD has been routinely planned 1 or 2 weeks earlier by our obstetric staff. This was due to the prevailing beliefs that women with previous cesarean delivery tend to develop labor at early term [18] and the outcome of pre-labor cesarean delivery is better than intrapartum cesarean deliveries [19]. Furthermore, some colleagues feared, though unjustifiable, that labor might cause uterine scar dehiscence/rupture [20], with all related potential medicolegal litigations [21].
Our findings are consistent with a study by Ganchimeg et al who enrolled 29,647 women in the WHO multi-country survey released in 2016 [15]. They excluded 35.9% of cases presenting in labor and compared only pre-labor cesareans at any given week with ongoing pregnancies and reported their findings. They concluded that the worse neonatal outcome was encountered at 37 weeks while there was no major difference in later weeks. On the other hand, no change of maternal outcomes was elicited with different scheduling times. In our cohort we could note that two factors were responsible for the occurrence of unplanned deliveries. It was obvious that spontaneous labor contributed to 80% while the emergence of obstetrical complications contributed to 20%. Furthermore, labor indirectly relocated more than 45% of ERCDs planned at 39 weeks to an earlier delivery date and the resultant neonatal outcome, hence, corresponded to that specific for the actual delivery gestational age.
Continuing pregnancy carries the risk of developing labor in addition to added obstetric complications. Such obstetric complications, which compel delivery irrespective of the scheduled date, are commonly overlooked in the process of scheduling for ERCD. Vilchez et al found in a cohort of 12,406 cases that while waiting for planned delivery at 39 weeks, 26% developed a complication/indication for cesarean and 12% arrived in labor for repeat cesarean [22]. In the expectant management group, neonatal risks of continuing pregnancy at 38 weeks and beyond were higher than those having their elective delivery at 38 weeks, though maternal complication did not differ. The rate of added obstetric complications was marginally higher than ours (26% vs. 20%) but unlike their results, the neonatal outcomes in our cohort were not negatively affected. This might be explained by the larger sample size of the earlier study.
Few studies analyzed all aspects of scheduling time on neonatal, maternal or delivery-related logistics. A study conducted in Thailand in 2012 by Lumluk et al in 830 cases matched our methodology. They found that scheduling at 39 weeks resulted in 52.2% emergency cesareans deliveries, higher postpartum hemorrhage together with low Apgar scores and higher NICU admission rates when compared with cases scheduled earlier and the difference was statistically significant [23]. The same group expanded their population to 1,221 patients in 2016 to include elective primary cesarean delivery and used the same methodology in assessing outcomes according to scheduled gestational age [14]. Similarly, they reported 41.2% of cases presenting with labor before scheduled date at 39 weeks, with no change in maternal outcome, although neonatal adverse outcome showed improvement when cesarean delivery was done electively starting at 38 weeks onwards. A randomized trial by Glavind et al at Denmark examined the outcome of 635 parturients delivered by cesarean section at 38 weeks in comparison to that of 637 delivered at 39 weeks. Using an intention-to-treat approach, they reported that the risk of adverse neonatal or maternal outcomes, or a maternal composite outcome was similar between the two groups [12]. The authors concluded that scheduling at 39 weeks did not result in reducing neonatal morbidities when compared with scheduling at 38 weeks. Subsequently, the same group, in a secondary analysis of their study, reported that scheduling caesarean section after 39 weeks leads to a 60% increase in unscheduled caesarean sections and a 70% increase in delivery outside regular work hours as compared to scheduling of the procedure prior to 39 weeks [13].
It has been nicely stated by Myers et al that it is unlikely that “one-size-fits-all recommendation” will be suitable for every woman planned to deliver at term, as those recommendations address only one aspect of a complex obstetric decision that involves multiple competing neonatal, maternal interests and hospital logistics [6]. We anticipate that those in low-risk group who are expected to respond positively to the implementation of such policies are those cases planned for elective induction of labor or elective primary cesarean section. On the other hand, cases with one or more previous cesarean deliveries or with other known factors that increase the risk of developing labor before planned cesareans with its related untoward effects should be considered as high-risk population and hence should be managed differently. In fact, Kennare et al and Taylor et al both provided clear evidence that patients with one previous cesarean delivery were at increased risk of developing preterm birth with related neonatal and maternal consequences when compared with those with previous vaginal delivery [18, 24].
Multiple repeat cesarean sections are linked to higher maternal morbidities and these tend to increase with the order of cesarean section in a continuous fashion [25]. A number of studies examined the outcome of parturients with two or more previous cesarean deliveries and found increased maternal and neonatal morbidities and recommended delivery prior to 39 weeks’ gestation [26-28]. Hart et al found that women with two previous cesarean deliveries were at higher risk to develop maternal and neonatal morbidities if pregnancy continued compared to their counterparts delivered at 38 weeks [26]. The authors suggested that women with two previous cesarean deliveries be scheduled at 38 + 0/7 - 38 + 6/7, while those with ≥ three previous cesarean deliveries be scheduled at 37 + 0/7 - 37 + 6/7. Lee et al in a decision-analysis model applied to a cohort of 200,000 cases of women with two prior cesarean deliveries found that delivery at 38 weeks as opposed to 39 weeks could prevent 94 stillbirths and was ultimately optimal as it maximized maternal and neonatal quality adjusted life years (QALYs) and concluded that delivery at 38 weeks’ gestation is the optimal time for women with two previous cesarean deliveries [27]. Finally, study by Melamed et al in a group of 377 patients with ≥ two previous cesarean deliveries reported an incidence of 26% of unplanned cesarean deliveries versus 13.3% at 39 and 38 weeks respectively and could find that scheduling a planned cesarean delivery at 39 weeks was associated with increased risk for maternal adverse outcome without apparent advantage in neonatal outcomes [28].
Whether delivery logistics (delivery at weekends, night shifts or outside regular working hours) could impact the outcome was the aim of a study by Peled et al, who reported the outcome of 9,944 unscheduled cesarean deliveries performed during three different work shifts [29]. They noted that delivery during night shift was associated with longer operative time and an increased risk for maternal, but not neonatal, morbidity.
Our study possessed a number of strengths. The study was possible due to the fact that patients were scheduled at three different times by their primary obstetrician rather than according to a single standardized institutional protocol, which allowed for the enrollment of subjects scheduled for delivery at 37, 38, and 39 weeks. Another feature of this group was its mixed-risk nature, where history of more than two cesarean deliveries was present in 37.4%, co-morbidities existed in 28.6%, 27.1% were smokers, 19.7% were obese, advanced maternal age ≥ 35 years in 21.2% and diabetes mellitus in 5.6%. On the other hand, the study had a number of limitations. The data were derived from a single center experience, and the small sample size limited our ability to analyze infrequent secondary outcomes. Finally, the inability to determine the duration of labor before admission deprived us of the ability to analyze its possible effect on the outcomes.
In conclusion, this study confirmed the superior neonatal outcome corresponding to delivery at 39 completed weeks when compared to 37 weeks’ gestation but was marginally better than the outcome at 38 weeks. No significant effect was elicited on maternal outcome, except the need to perform the delivery urgently and on weekends or at night shifts especially for those scheduled at 39 weeks. In fact, timing of ERCD is a delicate trade-off between neonatal and maternal interests, not to overlook the added risk of certain obstetric complications that may complicate ongoing pregnancies especially at or beyond 39 weeks of gestation. There is paucity of evidence-based information available to counsel patients with multiple previous cesarean deliveries concerning optimal timing of scheduling delivery. Hence, the urgent need for multicenter randomized controlled trials to clarify some hitherto unavailable risks/benefits linked to scheduling of ERCD. Individualizing patients, according to their risk of labor and added obstetrical complications, should be the initial step in scheduling process, especially when working at rural or small maternities and hospitals where blood banks, in-house anesthesia, laboratory services and adequate staffing might not be constantly available. We strongly believe that the conflict is not between neonatal and maternal interests, but is rather between scheduling at an optimal date and the ability to deliver at that exact date.
Acknowledgments
We are grateful to the immense contribution and the great work done by Ms. Loubna Sinno, the research coordinator at Makassed General Hospital.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Not applicable.
Author Contributions
None to declare.
| References | ▴Top |
- The American Academy of Pediatrics (AAP) Committee on Fetus and Newborn. Guidelines for perinatal care. 7th ed. ACOG Committee on Obstetric Practice; 2012: p. 193.
- van den Berg A, van Elburg RM, van Geijn HP, Fetter WP. Neonatal respiratory morbidity following elective caesarean section in term infants. A 5-year retrospective study and a review of the literature. Eur J Obstet Gynecol Reprod Biol. 2001;98(1):9-13.
doi - Tita AT, Landon MB, Spong CY, Lai Y, Leveno KJ, Varner MW, Moawad AH, et al. Timing of elective repeat cesarean delivery at term and neonatal outcomes. N Engl J Med. 2009;360(2):111-120.
doi pubmed - Wilmink FA, Hukkelhoven CW, Lunshof S, Mol BW, van der Post JA, Papatsonis DN. Neonatal outcome following elective cesarean section beyond 37 weeks of gestation: a 7-year retrospective analysis of a national registry. Am J Obstet Gynecol. 2010;202(3):250 e251-258.
- Ehrenthal DB, Hoffman MK, Jiang X, Ostrum G. Neonatal outcomes after implementation of guidelines limiting elective delivery before 39 weeks of gestation. Obstet Gynecol. 2011;118(5):1047-1055.
doi pubmed - Myers SA, Waters TP, Dawson NV. Fetal, neonatal and infant death and their relationship to best gestational age for delivery at term: is 39 weeks best for everyone? J Perinatol. 2014;34(7):503-507.
doi pubmed - Tita AT, Lai Y, Landon MB, Spong CY, Leveno KJ, Varner MW, Caritis SN, et al. Timing of elective repeat cesarean delivery at term and maternal perioperative outcomes. Obstet Gynecol. 2011;117(2 Pt 1):280-286.
doi pubmed - Chiossi G, Lai Y, Landon MB, Spong CY, Rouse DJ, Varner MW, Caritis SN, et al. Timing of delivery and adverse outcomes in term singleton repeat cesarean deliveries. Obstet Gynecol. 2013;121(3):561-569.
doi pubmed - Salim R, Shalev E. Health implications resulting from the timing of elective cesarean delivery. Reprod Biol Endocrinol. 2010;8:68.
doi pubmed - Allen VM, O'Connell CM, Liston RM, Baskett TF. Maternal morbidity associated with cesarean delivery without labor compared with spontaneous onset of labor at term. Obstet Gynecol. 2003;102(3):477-482.
pubmed - Hutcheon JA, Strumpf EC, Harper S, Giesbrecht E. Maternal and neonatal outcomes after implementation of a hospital policy to limit low-risk planned caesarean deliveries before 39 weeks of gestation: an interrupted time-series analysis. BJOG. 2015;122(9):1200-1206.
doi pubmed - Glavind J, Kindberg SF, Uldbjerg N, Khalil M, Moller AM, Mortensen BB, Rasmussen OB, et al. Elective caesarean section at 38 weeks versus 39 weeks: neonatal and maternal outcomes in a randomised controlled trial. BJOG. 2013;120(9):1123-1132.
doi pubmed - Glavind J, Henriksen TB, Kindberg SF, Uldbjerg N. Randomised trial of planned caesarean section prior to versus after 39 weeks: unscheduled deliveries and facility logistics—a secondary analysis. PLoS One. 2013;8(12):e84744.
doi pubmed - Phaloprakarn C, Tangjitgamol S, Manusirivithaya S. Timing of elective cesarean delivery at term and its impact on maternal and neonatal outcomes among Thai and other Southeast Asian pregnant women. J Obstet Gynaecol Res. 2016;42(8):936-943.
doi pubmed - Ganchimeg T, Nagata C, Vogel JP, Morisaki N, Pileggi-Castro C, Ortiz-Panozo E, Jayaratne K, et al. Optimal timing of delivery among low-risk women with prior caesarean section: a secondary analysis of the WHO multicountry survey on maternal and newborn health. PLoS One. 2016;11(2):e0149091.
doi pubmed - Bateman BT, Mhyre JM, Hernandez-Diaz S, et al. Development of a comorbidity index for use in obstetric patients. Obstet Gynecol. 2013;122:5.
doi pubmed - Davies GAL, Maxwell C, McLeod L, Maternal Fetal Medicine C, Clinical Practice O. Obesity in pregnancy. J Obstet Gynaecol Can. 2010;32(2):165-173.
doi - Kennare R, Tucker G, Heard A, Chan A. Risks of adverse outcomes in the next birth after a first cesarean delivery. Obstet Gynecol. 2007;109(2 Pt 1):270-276.
doi pubmed - Roberts CL, Nicholl MC, Algert CS, Ford JB, Morris JM, Chen JS. Rate of spontaneous onset of labour before planned repeat caesarean section at term. BMC Pregnancy Childbirth. 2014;14:125.
doi pubmed - Lydon-Rochelle M, Holt VL, Easterling TR, Martin DP. Risk of uterine rupture during labor among women with a prior cesarean delivery. N Engl J Med. 2001;345(1):3-8.
doi pubmed - Minkoff H. Fear of litigation and cesarean section rates. Semin Perinatol. 2012;36(5):390-394.
doi pubmed - Vilchez G, Chelliah A, Bratley E, Bahado-Singh R, Sokol R. Decreased risk of prematurity after elective repeat cesarean delivery in Hispanics. J Matern Fetal Neonatal Med. 2015;28(2):141-145.
doi pubmed - Lumluk T, Phaloprakarn C, Manusirivithaya S, Tangjitgamol S. Prevalence of spontaneous labor pain prior to scheduled cesarean section in pregnant women with previous uterine surgery. Vajira Med J. 2011;55(3):195-203.
- Taylor LK, Simpson JM, Roberts CL, Olive EC, Henderson-Smart DJ. Risk of complications in a second pregnancy following caesarean section in the first pregnancy: a population-based study. Med J Aust. 2005;183(10):515-519.
pubmed - Silver RM, Landon MB, Rouse DJ, Leveno KJ, Spong CY, Thom EA, Moawad AH, et al. Maternal morbidity associated with multiple repeat cesarean deliveries. Obstet Gynecol. 2006;107(6):1226-1232.
doi pubmed - Hart L, Refuerzo J, Sibai B, Blackwell S. Should the "39 week rule" apply to women with multiple prior cesarean deliveries? Am J Obstet Gynecol. 2014;210(1):S27.
doi - Lee V, Dorius A, Niu B, Griffin E, Kaimal A, Caughey A. Timing of delivery in women with two prior cesareans: a decision analysis. Am J Obstet Gynecol. 2015;212(1):S132.
doi - Melamed N, Hadar E, Keidar L, Peled Y, Wiznitzer A, Yogev Y. Timing of planned repeat cesarean delivery after two or more previous cesarean sections - risk for unplanned cesarean delivery and pregnancy outcome. J Matern Fetal Neonatal Med. 2014;27(5):431-438.
doi pubmed - Peled Y, Melamed N, Chen R, Pardo J, Ben-Shitrit G, Yogev Y. The effect of time of day on outcome of unscheduled cesarean deliveries. J Matern Fetal Neonatal Med. 2011;24(8):1051-1054.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
