| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website http://www.jcgo.org |
Case Report
Volume 9, Number 1-2, June 2020, pages 17-20
Proximal Hamstring Avulsion During Childbirth
Marya Ghazzia, b, c, Justin D. Stulla, Christopher J. Mehalloa, Christopher C. Dodsona
aRothman Orthopaedic Institute at Thomas Jefferson University, Philadelphia, PA 19107, USA
bPhiladelphia College of Osteopathic Medicine, Philadelphia, PA 19131, USA
cCorresponding Author: Marya Ghazzi, Rothman Orthopaedic Institute, 125 S 9th St. Ste 1000, Philadelphia, PA 19107, USA
Manuscript submitted March 28, 2020, accepted May 12, 2020, published online June 5, 2020
Short title: Proximal Hamstring Avulsion During Childbirth
doi: https://doi.org/10.14740/jcgo637
| Abstract | ▴Top |
Hormonal changes during pregnancy that increase soft tissue laxity and extreme body position during labor may predispose women to musculoskeletal injuries. This case describes a rare example of an acute proximal hamstring avulsion during childbirth. A 39-year-old female presented to the clinic with 2 weeks of right posterior thigh pain and bruising after the vaginal delivery of her infant. McRoberts’ maneuver was utilized during childbirth, which may have contributed to a proximal hamstring avulsion ultimately requiring surgical repair. Pregnant women may be at risk of tendinous injuries due to particular body positioning and concurrent hormonal changes. Special attention may be warranted in prenatal and perinatal women to avoid excessive stress on tendons, thus potentially preventing acute strain or rupture.
Keywords: Hamstring avulsion; Childbirth; Musculoskeletal injury
| Introduction | ▴Top |
Pregnancy is a time of immense physiological change across the body, and alterations to the musculoskeletal system certainly occur. Women often experience weight gain, shifts in weight distribution, and soft tissue laxity resulting from a variety of hormonal changes. The hormone relaxin plays a significant role in these musculoskeletal changes; it is primarily responsible for soft tissue laxity [1]. While these systemic changes aid in fetal development and prepare the mother for childbirth, they can also predispose women to injury. We present a case of an acute hamstring avulsion during childbirth as an example of such an injury.
Acute proximal hamstring rupture occurs most often as a result of sudden contraction of the hamstrings secondary to extreme hip flexion with knee extension. The greatest risk factor for hamstring rupture is previous strain or injury; however, there is a correlation between age, flexibility, and other factors that can predispose an individual to acute rupture [2]. More specifically, there are several elements of childbirth that can potentially place a woman at risk of hamstring rupture during delivery such as body positioning with deep flexion (i.e., McRoberts’ maneuver), age, and possible muscle deconditioning due to less physical activity during pregnancy.
There is limited published information regarding tendinous changes and associated risk of tendinous injury during pregnancy. To our knowledge, there are no previous case reports of acute hamstring rupture during childbirth. Thus, this case report describes a unique presentation for a proximal hamstring avulsion sustained during an otherwise uncomplicated vaginal delivery.
| Case Report | ▴Top |
A 39-year-old postpartum female presented to the orthopedic clinic for evaluation of right thigh pain and bruising. The symptoms had been present for 2 weeks, first noticed after the vaginal delivery of her infant. During delivery, McRoberts’ maneuver was utilized to assist with the anatomic barriers of childbirth. In this position, the hips are placed in a position of hyperflexion. The patient stated that during an episode of pushing, she and other witnesses in the room heard a loud pop. The patient denied any immediate pain, but noted she had an epidural for analgesia during delivery. On day 2 of her hospital visit, she noticed posterior thigh bruising along with the development of posterior thigh pain and weakness. Over the following 2 weeks, the patient continued to develop significant pain and bruising on the posterior right thigh into the posterior right calf. She denied any numbness or tingling.
On examination, the patient was a healthy appearing female in no acute distress. She was 68 kg and 164 cm with a body mass index (BMI) of 25.3. Evaluation of her right lower extremity demonstrated significant posterior thigh ecchymosis and a palpable defect of the proximal hamstring tendon. She had a positive tripod test, indicating decreased hamstring extensibility. In a tripod test, the patient is seated with the knees flexed over the edge of the table; the practitioner passively extends the knee while looking for any changes in position of the patient’s trunk. A positive test is represented by increased trunk extension. The patient also exhibited significant hamstring weakness, along with pain in the posterior thigh musculature with right lower extremity movement. She was neurovascularly intact distally. Both the thigh and calf compartments were soft and nontender. Radiographs of her bilateral hips showed a cam type of impingement with a moderate degree of osteoarthritis (Fig. 1). Magnetic resonance imaging (MRI) without contrast of her pelvis and right thigh showed an acute avulsion of the right proximal hamstring conjoint tendon, with distal retraction by approximately 6 cm. MRI also revealed a 4.6 × 3.6 × 10.7 cm intramuscular hematoma in the hamstring and bilateral mild hip arthritis (Figs. 2, 3).
 Click for large image | Figure 1. The X-ray image of pelvis, AP view, showing cam-type impingement and moderate osteoarthritis. AP: anteroposterior. |
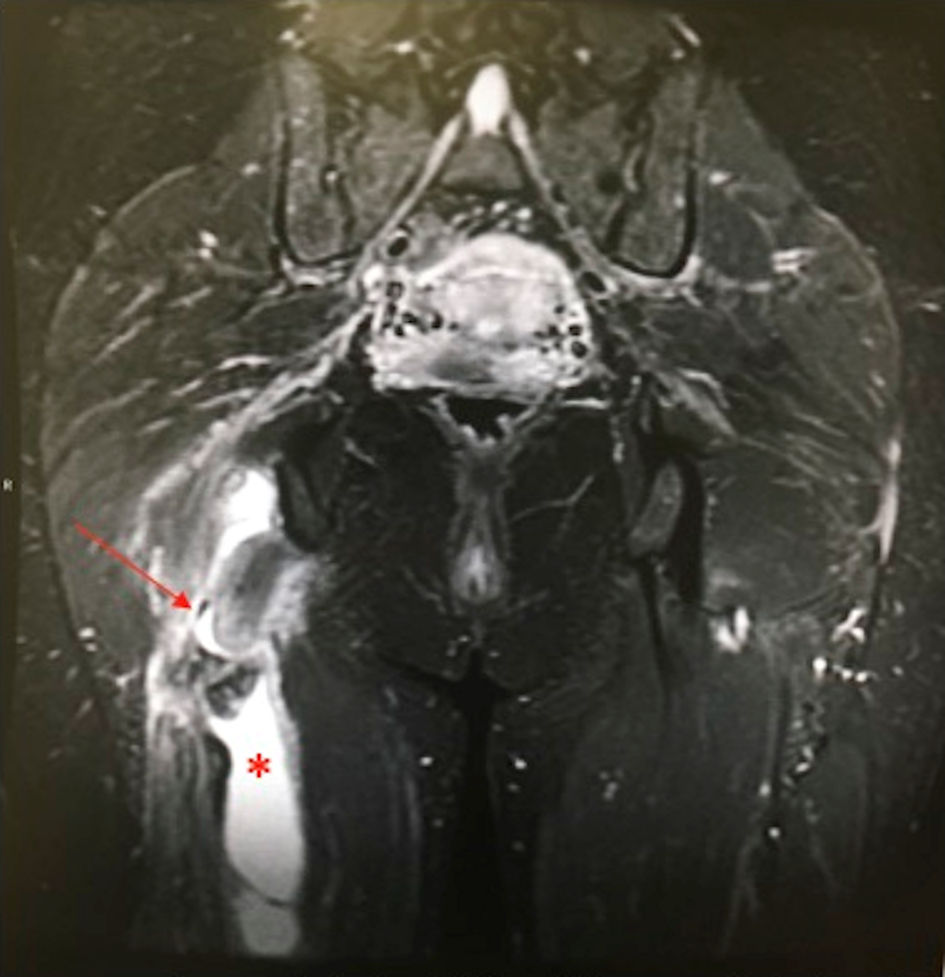 Click for large image | Figure 2. The magnetic resonance image of pelvis and right thigh, coronal STIR view, showing an acute avulsion of the right proximal hamstring conjoint tendon (red arrow) with distal retraction by 6 cm, and a 4.6 × 3.6 × 10.7 cm intramuscular hematoma in the hamstring (asterisk). |
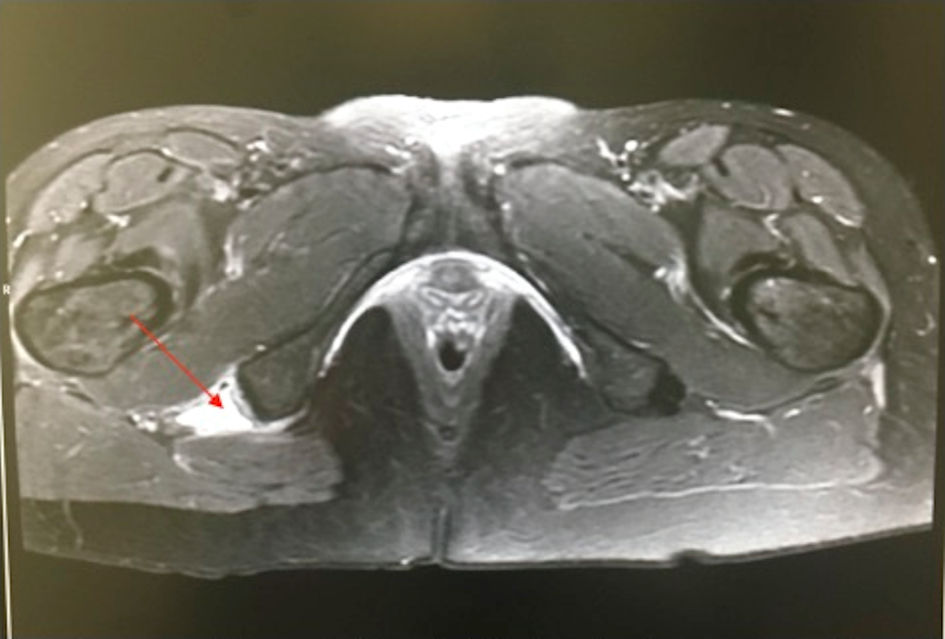 Click for large image | Figure 3. The magnetic resonance image of pelvis, axial STIR view, showing an acute avulsion of the proximal hamstring conjoint tendon (red arrow). |
The patient was diagnosed with a complete proximal hamstring avulsion and referred to an orthopedic surgeon for a hamstring repair. The risks and benefits of surgery were discussed, and the patient proceeded with surgery. Postoperatively, the patient was non-weight bearing and placed in a right hip abduction brace to be worn all the time. She was seen for follow-up at 2, 6, 12, and 24 weeks. At 2 weeks, she could begin weight bearing with crutches and was instructed to start physical therapy. At 6 weeks, she discontinued the brace and crutches. At 12 weeks, she was walking with normal gait but had slight weakness in her hamstring strength. At 24 weeks, she had a normal tripod test and 5/5 hamstring strength. She was cleared to resume normal activities at this time.
| Discussion | ▴Top |
Childbirth is a traumatic process, in which both the mother and infant are at risk for musculoskeletal injuries. While maternal orthopedic injuries during childbirth have been reported in small numbers, most have focused on structures within the pelvic ring such as the sacroiliac joint and pubic symphysis [1]. This case describes a maternal injury to the hamstring, which we believe is correlated with body positioning and simultaneous hormonal changes that increased the probability of hamstring rupture during labor.
Extreme body positioning may cause abrupt increases in tendon load, thus putting the tendon at risk of rupture. McRoberts’ maneuver, a technique used in the case of shoulder dystocia during childbirth, involves placing the mother in such extreme positioning. In this procedure, the mother’s feet are pushed cephalad, causing hyperflexion of the mother’s hips and knees. Extension of the mother’s knees from this position could rapidly increase eccentric load across the myotendinous unit of the hamstring. While using this maneuver has been previously described as a risk factor for maternal injuries to the pelvic ring [3], its association with other maternal orthopedic injuries is not well documented. The use of McRoberts’ maneuver in this case may have been a significant contributing factor in creating a rapid hamstring load, increasing the possibility of rupture. Maintaining knee flexion during the maneuver may decrease eccentric load on the tendon and thus reduce this risk.
Although there are risks associated with positioning, we should not discount the hormonal influence that may further predispose pregnant women to musculoskeletal injuries. There have been reports of soft tissue injuries, including ligamentous and tendinous injuries, under the effect of certain hormones in the pregnant patient. Relaxin is one such hormone; it promotes the dissociation of collagen fibrils and is increased during pregnancy. Thus, an increase in relaxin would be expected increase the laxity of tendons through the activation of collagenase [4]. However, relaxin also decreases the tendon fibril diameter and organization [5], potentially increasing the risk of rupture. In addition to relaxin, there are other hormones that may contribute to a greater possibility of soft tissue injury. Generally, estrogen is expected to cause laxity of tendon and therefore decrease the incidence of injury to associated muscles. While data suggest that the periodic rise in estrogen may provide a protective effect on tendons, sustained high levels of estrogen as in pregnancy could have a negative impact. Studies have shown that in premenopausal women on oral contraceptives, a consistent moderate elevation in estrogen levels resulted in decreased collagen synthesis. Conversely, estrogen replacement therapy in postmenopausal women, which provides a daily moderate rise in estrogen, resulted in increased tendon collagen synthesis [6]. Moreover, elevated estrogen levels during pregnancy can increase immunosuppression, which may negatively impact collagen production [7]. These data suggest that the sustained elevation of estrogen levels during pregnancy could contribute to the increased risk of tendon injury. Other potential hormonal influences during pregnancy include substance P and cortisol. Decreases in substance P levels, which occur in pregnant women, have been associated with delayed tendinopathy healing in an animal model [8]. Hypercortisolism is a byproduct of pregnancy due to the production of corticotropin-releasing hormone (CRH) and adrenocorticotropic hormone (ACTH), and this state of increased glucocorticoids is a risk factor for tendon rupture [9]. Overall, it is important to note the potential significance of hormonal influence along with body positioning as contributory factors in this case.
This case also highlights possible broader implications to women’s musculoskeletal health during pregnancy. The potential increased risk of injury due to body positioning and hormonal variations may extend to the prenatal period in addition to childbirth. For example, while prenatal yoga and exercise can have a positive impact on a woman’s well-being throughout pregnancy, body and limb positioning should be carefully considered to minimize the risk of injury. Current evidence suggests that relaxin levels are increased throughout pregnancy and peak at week 12 of gestation [1]. The effect of relaxin on tendon fiber diameter and organization [5] could possibly increase the risk of tendon rupture during this time. However, given the limited available evidence, additional studies may be warranted to better elucidate the potential increased susceptibility to musculoskeletal injury during the prenatal period.
While we acknowledge the novelty of this case report, we believe that it represents an opportunity to recognize the potential increased chance of musculoskeletal injury during pregnancy and specifically delivery. Hormonal shifts in the pre and perinatal periods, in concert with particular body positioning, may have a significant impact on the chance of tendinous injury. Although prompt surgical intervention resulted in a favorable outcome for our patient, such injuries could be prevented with greater awareness of these risks and strategies to mitigate them. For example, eccentric training using a home exercise program could prevent rapid eccentric loading on tendons. Avoiding certain positions, such as knee extension during the McRoberts’ maneuver, could also play an important role in preventing tendinous injuries. In conclusion, close attention should be given to body positioning of the pregnant patient, especially during the childbirth process.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Written patient consent for publication has been obtained.
Author Contributions
JDS wrote the first draft. MG wrote the second draft and completed all edits for revision and submission. CJM was one of the treating physicians and reviewed/edited all manuscripts. CCD was one of the treating physicians and reviewed the first manuscript.
Data Availability
The authors declare that the data supporting the findings of this study are available within the article.
| References | ▴Top |
- Borg-Stein J, Dugan SA, Gruber J. Musculoskeletal aspects of pregnancy. Am J Phys Med Rehabil. 2005;84(3):180-192.
doi pubmed - Lempainen L, Banke IJ, Johansson K, Brucker PU, Sarimo J, Orava S, Imhoff AB. Clinical principles in the management of hamstring injuries. Knee Surg Sports Traumatol Arthrosc. 2015;23(8):2449-2456.
doi pubmed - Heath T, Gherman RB. Symphyseal separation, sacroiliac joint dislocation and transient lateral femoral cutaneous neuropathy associated with McRoberts' maneuver. A case report. J Reprod Med. 1999;44(10):902-904.
- Dehghan F, Haerian BS, Muniandy S, Yusof A, Dragoo JL, Salleh N. The effect of relaxin on the musculoskeletal system. Scand J Med Sci Sports. 2014;24(4):e220-229.
doi pubmed - Blecher AM, Richmond JC. Transient laxity of an anterior cruciate ligament-reconstructed knee related to pregnancy. Arthroscopy. 1998;14(1):77-79.
doi - Chidi-Ogbolu N, Baar K. Effect of estrogen on musculoskeletal performance and injury risk. Front Physiol. 2018;9:1834.
doi pubmed - Bhatti A, Hussain A, Ragoowansi R. Flexor pollicis longus rupture during pregnancy following previous primary repair. J Hand Surg Eur Vol. 2010;35(4):326-327.
doi pubmed - Hart DA, Kydd A, Reno C. Gender and pregnancy affect neuropeptide responses of the rabbit Achilles tendon. Clin Orthop Relat Res. 1999;365:237-246.
doi pubmed - Galdiero M, Auriemma RS, Pivonello R, Colao A. Cushing, acromegaly, GH deficiency and tendons. Muscles Ligaments Tendons J. 2014;4(3):329-332.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
