| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website https://www.jcgo.org |
Review
Volume 9, Number 3, September 2020, pages 31-36
Could Laparoscopic Concerns During Coronavirus Pandemic Affect the Care of Women With Pregnancy of Unknown Location/Ectopic Pregnancy?
Sofia F. Makrydimaa, c, Dorothea Saraglib
aGynecological Oncology, Barking, Havering and Redbridge (BHR) University Hospitals, Romford, Essex, UK
bAmbulatory Gynecology in St Helier Hospital (Epsom and St Helier University Hospitals), Sutton, Carshalton, UK
cCorresponding Author: Sofia F. Makrydima, Gynecological Oncology, Barking, Havering and Redbridge (BHR) University Hospitals, Romford, Essex, UK
Manuscript submitted June 8, 2020, accepted August 12, 2020, published online September 9, 2020
Short title: PUL Management During COVID-19
doi: https://doi.org/10.14740/jcgo657
- Abstract
- Introduction
- Evidence of Viruses/Bacteria Presence in Pneumoperitoneum
- Evaporation/Sublimation of Infected Tissues is not Unique for Laparoscopy
- Can Coronavirus Be Found in Blood, Abdominal Tissues or Bodily Fluids? Can It Be Transmitted Through Contact With These Tissues? Does It Exist in the Pneumoperitoneum?
- Management of Patients in Need of Emergency Laparoscopic Surgery Should Be Individualized
- Coronavirus Pandemic-Associated Dilemmas in the Management of Symptomatic Women With Pregnancy of Unknown Location/Suspected Ectopic Pregnancy
- Safety Precautions During Laparoscopy
- Conclusions
- References
| Abstract | ▴Top |
In the coronavirus pandemic elective surgery has been deferred and therefore emergency surgery for suspected ectopic pregnancy arises as the most commonly performed operation in gynecology. Laparoscopic management has traditionally been the gold standard, however recently concerns have been raised regarding severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) dissemination as aerosolized small particles are presumed to escape abdominal cavity. The rationale for this hypothesis is based on cohort studies confirming presence of blood-borne viruses such as human immunodeficiency virus (HIV) and hepatitis B virus (HBV) in the surgical plume, whereas data for airborne viruses such as SARS-CoV-2 are scarce. Remarkably, there is no solid evidence up to date to associate inhalation of pneumoperitoneum viral particles with subsequent disease of theatre staff. Reverse transcription-polymerase chain reaction (RT-PCR) on blood samples of coronavirus disease 2019 (COVID-19)-infected patients presenting with fever, confirmed viremia in only 1% of cases. The viral ribonucleic acid (RNA) was isolated in stool samples in 29% of cases but was not found in urine samples. Therefore, the use of surgical energy devices on genital tract tissues bears little chance of producing aerosolized COVID-19 particles. The optimal surgical approach should be individualized according to a variety of factors: complexity of case and bowel involvement, length of procedure, comorbidities, hospital stay, as well as the surgeon’s familiarity with each approach. When necessary precautions are taken, laparoscopy for ectopic pregnancy appears safe. Operating theatres should meet technical specifications and maintain negative pressure if possible. Only essential personnel equipped with personal protective equipment should be attending theatres. Abdominal pressure should be set under 12 mm Hg and ultrasonic/bipolar device use minimized. Smoke evacuation filtration systems and disposable trocars with insufflation taps can contain surgical smoke. As more information is emerging, trusts will adjust to evolving circumstances with standard operating procedures. Changing established practice may be premature as clinicians should “first do no harm”.
Keywords: Coronavirus; Laparoscopy; Ectopic pregnancy
| Introduction | ▴Top |
It has recently been reported that 20% of health care workers in Italy have been infected by coronavirus, which understandably has created anxiety among the scientific community [1]. We have now seen at least 180 doctors and nurses dying in the UK. Undoubtedly, access to appropriate personal protective equipment (PPE) remains the cornerstone of the problem.
Among other key issues, concerns have been raised regarding the risk of severe acute respiratory syndrome (SARS) that might be caused due to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) dissemination during minimally invasive surgery. Pneumoperitoneum-related aerosolized small particles containing the virus ribonucleic acid (RNA) are presumed to escape from the abdominal cavity, due to pressure difference, and can subsequently be inhaled by theatre staff. Steps of particular relevance include retrieval of surgical specimens, as well as the final desufflation of the abdominal cavity. Small particles are also likely to escape around the port sites or through the trocars when inserting and removing laparoscopic instruments. Obviously, this possibility is directly proportional to the abdominal pressure maintained throughout the procedure as well as the complexity and length of each case.
However, during the coronavirus disease 2019 (COVID-19) pandemic, all elective surgeries have been deferred, with the exception of suspected cancer cases. This policy was introduced in an effort to minimize the spread of the virus, but also in order to increase availability of staff and equipment, e.g., ventilators, intensive care unit (ICU) beds. In regard to emergency gynecological surgery, surgical management of incomplete miscarriage has been largely substituted by manual vacuum aspiration (MVA). Consequently, emergency surgery for suspected/confirmed ectopic pregnancy, which is traditionally laparoscopic, may currently be the most commonly performed operation in gynecology.
| Evidence of Viruses/Bacteria Presence in Pneumoperitoneum | ▴Top |
The rationale of the hypothesis of coronavirus aerosolization during laparoscopy was based on studies on blood-borne viruses, such as hepatitis B virus (HBV) and human immunodeficiency virus (HIV). In 2016, a Korean study proved the existence of HBV in surgical smoke in 10 out of 11 patients undergoing laparoscopic colorectal procedures [2]. HIV-1 can remain viable in cool aerosols generated by certain surgical power tools that raises the possibility of HIV transmission to medical personnel exposed to aerosols, similarly, generated during the care of HIV-infected patients [3].
An outbreak of group A Streptococcus (GAS) has been reported in a hospital, after highlighting two cases that underwent uncomplicated laparoscopic surgery in the same operating room [4]. GAS is a traditional skin-to-skin/mucosa-to-mucosa transmitted pathogen. None of the 46 members of the staff that came in contact with these patients were found to be colonized with the same strain of GAS. Infection control investigation concluded that aerosolization of particles from the first patient was the most possible source of transmission, despite the lack of definite evidence.
It is crucial to highlight that there are limited data regarding classical airborne infections. There are case reports of port sites tuberculosis following laparoscopy. However, they were associated with poor disinfection between theatre cases, as none of the patients exhibited clinical signs of tuberculosis perioperatively [5]. Bioaerosol produced at low temperature as in harmonic scissors may contain live multidrug resistant Mycobacterium tuberculosis [6].
| Evaporation/Sublimation of Infected Tissues is not Unique for Laparoscopy | ▴Top |
Notably, the fact that production of surgical smoke constitutes an occupational health hazard has not come as a surprise to the scientific community [7]. The inhalation of airborne particles has not only been associated with transmission of infections, but also with upper respiratory tract irritation and possible carcinogenesis. Surgical smoke is produced by the use of energy devices and as such, it is not unique for laparoscopic surgery. In fact, as experienced surgeons argue, better containment and filtration of the surgical gas and plume can be achieved by laparoscopy compared to laparotomy, as a closed system can be designed [8].
Human papillomavirus (HPV) deoxyribonucleic acid (DNA) has been found in surgical smoke in 29.9% of cases undergoing cervical loop electrosurgical excision procedures (LEEP). The positive rate of HPV DNA in surgical smoke was significantly increased for greater distances of the suction device from the surgical site. Flow fluorescence in situ hybridization on nasal epithelial cells of the surgeons detected HPV DNA in 1.5% of them (2 out of 134). After a 3 - 6-month follow-up, the nasal swabs from these two doctors tested negative for HPV DNA [9]. Greater amounts of HPV DNA were usually recovered in the laser vapor (carbon dioxide (CO2)) compared to the electrocoagulation vapor produced during treatment of human plantar warts [10].
Poliovirus, which is classified as airborne virus, has been detected in the smoke produced by ablation of infected fibroblasts using excimer laser [11].
Electrosurgery generates the smallest particles with a mean diameter of 0.07 µm, laser-generated particles are typically larger up to 0.31 µm, while the ultrasonic scalpel by-products are the largest, with particle diameters ranging from 0.35 to 6.5 µm [12]. Traditional surgical masks are able to capture particles greater than 5 µm and as such they offer no protection against particles produced by electrosurgical and laser devices. Therefore, systems for continuous smoke evacuation have been implemented [13].
Taken together, it can be deduced that the sole advantage of open surgery, in terms of preventing transmission of a virus during a pandemic, lies in the ability to minimize or completely avoid the use of any energy devices. This needs to be balanced against the standard risks of open surgery, such as needle stick injury [14] and contact with other bodily fluids, as well as the impact on the patient due to longer hospital stay. A summary of relevant studies is displayed in Table 1 [2-6, 9-11, 15].
 Click to view | Table 1. Summary of Available Studies Regarding Presence of Bacteria/Viruses in Surgical Smoke and Transmission of Relevant Infections |
| Can Coronavirus Be Found in Blood, Abdominal Tissues or Bodily Fluids? Can It Be Transmitted Through Contact With These Tissues? Does It Exist in the Pneumoperitoneum? | ▴Top |
It needs to be stressed that up to date there is no study to report presence of coronavirus RNA in pneumoperitoneum of infected patients. But even if presence was to be confirmed in the future, it wouldn’t necessarily mean that it can cause clinical infection as it may not be in sufficient amount or appropriate form.
Interestingly, reverse transcription-polymerase chain reaction (RT-PCR) on blood samples of COVID-19-infected patients presenting with fever, confirmed viremia in only 1% of cases. Furthermore, as expected for an airborne virus that can be swallowed and carried through the gastrointestinal tract, it was present in stool samples in 29% of cases. Coronavirus RNA was not detected in any of the urine samples taken from 72 patients [16]. Vertical transmission of SARS-CoV-2 has not been detected, although perinatal transmission was suspected in one case [17]. Thus, the theoretical risk of presence of coronavirus particles in the pneumoperitoneum of patients undergoing gynecological surgery, appears to be negligible, except for cases where bowel is involved.
SARS-CoV-2 is an RNA virus that has a size range of 0.06 to 0.14 µm [18]. All respiratory viruses normally attach to receptors in the airways (with the exception of adenoviruses) and therefore the feasibility of blood-borne transmission of respiratory viruses is unlikely. At this point, it should be highlighted that no transmissions by blood or other substances of human origin have been documented or alleged for novel coronavirus (2019-nCoV). Interestingly, this is in consistency with data for the other two coronaviruses that have emerged over the past two decades (SARS-CoV and MERS-CoV, causing Mideast respiratory syndrome) [19].
| Management of Patients in Need of Emergency Laparoscopic Surgery Should Be Individualized | ▴Top |
While the surgical approach remains controversial for the scientific community, it becomes apparent that management of the patients should be individualized. Coronavirus status could possibly be taken into consideration, whenever available, but the sensitivity of a single PCR swab (nasal/throat) does not exceed 63%. However, as the influx of coronavirus patients is increasing, every emergency case has to be treated as positive, until proven otherwise. Symptoms and contact questionnaires may be more relevant for the triage of semi- elective cases operated under the green pathway.
Most scientific societies addressed the concerns, assessed evolving evidence and released joint statements that endorsed laparoscopic approach, at least for procedures that do not involve the bowel [20]. In an effort to focus on surgical exposure, anesthetic considerations are commonly underemphasized, even though airway manipulation is the classical aerosol generating process. Intubation and extubation of the patient are by far the riskiest interventions and therefore spinal anesthesia may be an alternative for gynecological laparotomies or certain minimally invasive cases, e.g., hysteroscopies, large loop excision of the transformation zone (LLETZ) and surgical evacuation of products of conception.
Thus, the most essential parameter to acknowledge may be the type of surgery as well as the surgeon’s expertise that will affect the exposure time. In the specific case of suspected or confirmed ectopic pregnancy the patient is offered diagnostic laparoscopy ± unilateral salpingectomy/salpingotomy. Most commonly, this is a very quick procedure with minimal use of electrosurgical devices, which can even be performed using low abdominal pressure (under 12 mm Hg). In the rare cases of technically difficult procedure due to unexpected findings, e.g., abdominal adhesions, cesarean scar/interstitial/cornual pregnancy, laparoscopy is typically abandoned and converted to laparotomy.
| Coronavirus Pandemic-Associated Dilemmas in the Management of Symptomatic Women With Pregnancy of Unknown Location/Suspected Ectopic Pregnancy | ▴Top |
The management of pregnancy of unknown location/ ectopic pregnancy has been established by high quality papers. However, there are specific groups of patients that may be affected by coronavirus associated concerns and the possible reluctancy of clinicians to proceed with intervention. Indeed, a recent observational study from a university hospital in Bologna found that the rate of ruptured ectopic pregnancies in the coronavirus pandemic lockdown increased significantly [21].
Symptomatic patients presenting with severe abdominal pain and bleeding would normally be offered a diagnostic laparoscopy when scan findings are inconclusive. Depending on the unit, up to 30% of these patients will not have an ectopic pregnancy [22], which poses a clinical dilemma that becomes even greater under the current circumstances. On one hand, open procedure would be debatable with these high rates of negative findings, especially when we take into account that the patient will have to undergo an unnecessary hospital stay during coronavirus pandemic. On the other hand, missing the diagnosis of an ectopic pregnancy can have detrimental effects caused by rupture of the ectopic pregnancy and hemorrhagic shock. Some of these patients will be subjected to long hospital stay due to uncertainty regarding optimal management.
Anyhow, systematic reviews of case series of pregnant women undergoing surgical procedures in pregnancy have shown that laparotomy and laparoscopy are both safe and have similar obstetric outcomes. An increased ratio of fetal loss after laparoscopy has been attributed to its preferential use in early pregnancy, when the possibility of miscarriage is higher [23].
In another group of patients, the ones with minor symptoms and pregnancy of uncertain viability with scan findings favoring ectopic pregnancy, a diagnostic laparoscopic procedure +/- treatment of ectopic pregnancy or conservative follow up would be offered, according to patient’s preferences, set clinical criteria, e.g., blood human chorionic gonadotropin (hCG) levels, presence of free peritoneal fluid and inert characteristics, e.g., language barrier, committed to follow up patient. In the coronavirus pandemic, when by definition there is a need to reduce hospital attendances and unnecessary semi-elective interventions, methotrexate administration appears tempting. It is a mild immunosuppressive medication, but it is unlikely to cause vulnerability to COVID-19 at the dose used to treat ectopic pregnancy and it does not require shielding [24]. However, as doctors we should “first do no harm” and have zero tolerance for mistakenly diagnosing miscarriage, or ectopic pregnancy in cases where very early and viable intrauterine pregnancy exists [25]. In this sense, methotrexate should be strictly reserved for cases of persistent pregnancy of unknown location after excluding viability or in cases where an ectopic pregnancy that fulfils criteria for medical management is confirmed. We propose the algorithm depicted in Figure 1 for the management of suspected ectopic pregnancy during the coronavirus pandemic.
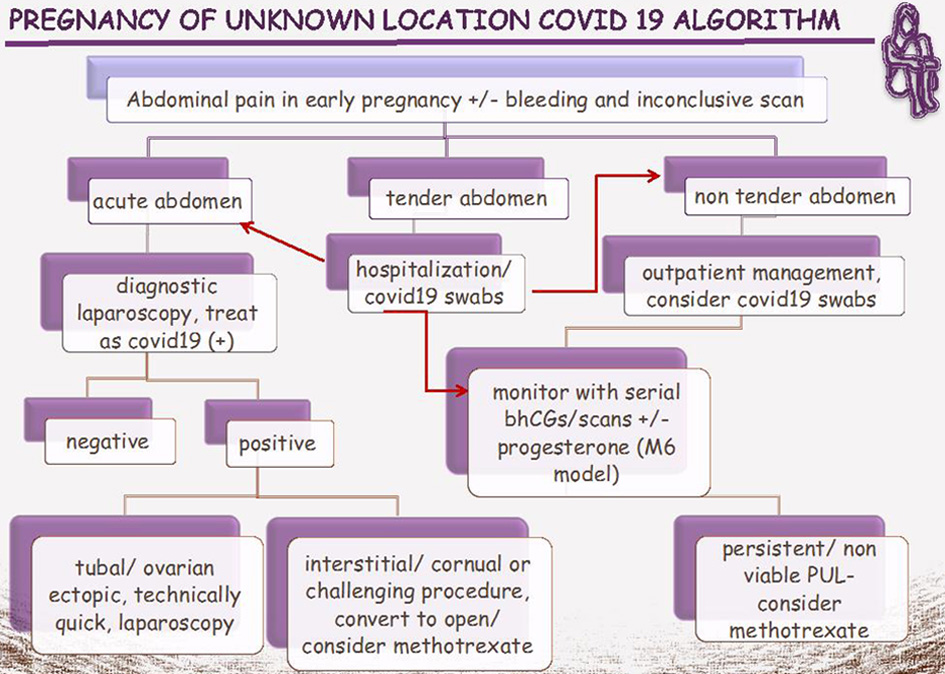 Click for large image | Figure 1. Proposed algorithm for the management of PUL during COVID-19 pandemic. COVID-19: coronavirus disease 2019; PUL: pregnancy of unknown location; bhCG: blood human chorionic gonadotropin. |
| Safety Precautions During Laparoscopy | ▴Top |
There is a fine balance between safety of all theatre staff and safety of the patient. Local protocols fitted to population characteristics and staff expertise may be relevant and should be encouraged. Regardless of the chosen approach, all necessary precautions should be in place to reduce the chance of exposure. Operating theatres should meet technical specifications; ideally, they could be converted to negative pressure rooms, so that airborne contaminants are contained within the room. This offers optimal protection to staff working in adjacent areas [26]. It can be achieved with the incorporation of a much stronger low-level exhaust system, which leads to a downward extraction of air. The vertical airflow stream is presumed to make infectious particles flow below the operating table until being drawn out of the room via the exhaust grilles. This means that surgical staff are at little risk of being infected by the patient during the operation. Heating, ventilation, air-conditioning (HVAC) systems perform multiple functions simultaneously, including controlling at least three known central variables in the airborne transmission of infectious particles: temperature, relative humidity and air currents. With regard to ventilation, various international scientific organizations, including Centers for Disease Control and Prevention (CDC), recommend a minimum of 15 - 20 air exchanges per hour, 3 - 4 (20%) of which must be fresh air [27]. Only essential personnel should be attending theatres and they should all be equipped with appropriate PPE. When available, a closed smoke evacuation/filtration system with ultra-low particulate air (ULPA) filtration capability should be employed. Skin incisions should be small, and trocars ideally have insufflation tap, so as to eliminate leakage of CO2 through port sites. Serving the same rationale, instrument diameter should fit the trocar, e.g., don’t use 5-mm camera through 12-mm trocar. Electrosurgical and ultrasonic scalpels should be used with caution and in a manner that minimizes production of plume, with low power setting and avoidance of long desiccation times. A trocar’s one-way valve is recommended to be attached to suction’s tube through filters in order to remove surgical plume during use of energy to prevent blurred imaging. Specimens should be retrieved in endobag following active desufflation of pneumoperitoneum with closed smoke evacuation/filtration system or laparoscopic suction. This practice will also diminish blood/fluid droplet spray or spread [28].
| Conclusions | ▴Top |
It appears necessary to adapt laparoscopic practice to the evolving circumstances as the coronavirus may be part of the everyday life possibly for the next few months if not years. As more information is emerging, our understanding of the virus biology will shed light to the optimal care for surgical emergencies. Until then, changing established management may be premature reaction and therefore international societies have not altered their published recommendation algorithms on ectopic pregnancy during coronavirus pandemic. Medical treatment remains the standard of care and surgical intervention should be undertaken when clinically indicated.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Author Contributions
Sofia F. Makrydima perceived the idea, edited and reviewed the manuscript. Dorothea Saragli edited and reviewed the manuscript.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- The Lancet. COVID-19: protecting health-care workers. Lancet. 2020;395(10228):922.
doi - Kwak HD, Kim SH, Seo YS, Song KJ. Detecting hepatitis B virus in surgical smoke emitted during laparoscopic surgery. Occup Environ Med. 2016;73(12):857-863.
doi pubmed - Johnson GK, Robinson WS. Human immunodeficiency virus-1 (HIV-1) in the vapors of surgical power instruments. J Med Virol. 1991;33(1):47-50.
doi pubmed - Al-ajmi JA, Hill P, C OB, Garcia ML, Malkawi M, George A, Saleh F, et al. Group A Streptococcus Toxic Shock Syndrome: An outbreak report and review of the literature. J Infect Public Health. 2012;5(6):388-393.
doi pubmed - Ramesh H, Prakash K, Lekha V, Jacob G, Venugopal A, Venugopal B. Port-site tuberculosis after laparoscopy: report of eight cases. Surg Endosc. 2003;17(6):930-932.
doi pubmed - Chowdhury KK, Meftahuzzaman SM, Rickta D, Chowdhury TK, Chowdhury BB, Ireen ST. Electrosurgical smoke: a real concern. Mymensingh Med J. 2011;20(3):507-512.
- Choi SH, Kwon TG, Chung SK, Kim TH. Surgical smoke may be a biohazard to surgeons performing laparoscopic surgery. Surg Endosc. 2014;28(8):2374-2380.
doi pubmed - Morris SN, Fader AN, Milad MP, Dionisi HJ. Understanding the "Scope" of the problem: why laparoscopy is considered safe during the COVID-19 pandemic. J Minim Invasive Gynecol. 2020;27(4):789-791.
doi pubmed - Zhou Q, Hu X, Zhou J, Zhao M, Zhu X, Zhu X. Human papillomavirus DNA in surgical smoke during cervical loop electrosurgical excision procedures and its impact on the surgeon. Cancer Manag Res. 2019;11:3643-3654.
doi pubmed - Sawchuk WS, Weber PJ, Lowy DR, Dzubow LM. Infectious papillomavirus in the vapor of warts treated with carbon dioxide laser or electrocoagulation: detection and protection. J Am Acad Dermatol. 1989;21(1):41-49.
doi - Taravella MJ, Weinberg A, May M, Stepp P. Live virus survives excimer laser ablation. Ophthalmology. 1999;106(8):1498-1499.
doi - Addley S, Quinn D. Surgical smoke - what are the risks? The Obstetrician & Gynaecologist. 2019;21:102-106.
doi - Fencl JL. Guideline implementation: surgical smoke safety. AORN J. 2017;105(5):488-497.
doi pubmed - Fry DE. Reduction of HIV transmission during laparoscopic procedures. Surg Laparosc Endosc. 1993;3(1):1.
- Capizzi PJ, Clay RP, Battey MJ. Microbiologic activity in laser resurfacing plume and debris. Lasers Surg Med. 1998;23(3):172-174.
doi - Wang W, Xu Y, Gao R, Lu R, Han K, Wu G, Tan W. Detection of SARS-CoV-2 in Different Types of Clinical Specimens. JAMA. 2020.
doi - Chen H, Guo J, Wang C, Luo F, Yu X, Zhang W, Li J, et al. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Lancet. 2020;395(10226):809-815.
doi - Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, Zhao X, et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N Engl J Med. 2020;382(8):727-733.
doi pubmed - Update: Impact of 2019 Novel Coronavirus and Blood Safety. http://www.aabb.org/advocacy/regulatorygovernment/Documents/Impact-of-2019-Novel-Coronavirus-on-Blood-Donation.pdf.
- Joint RCOG/BSGE Statement on gynaecological laparoscopic procedures and COVID-19. https://www.bsge.org.uk/news/joint-rcog-bsge-statement-on-gynaecological-laparoscopic-procedures-and-covid-19.
- Casadio P, Youssef A, Arena A, Gamal N, Pilu G, Seracchioli R. Increased rate of ruptured ectopic pregnancy in COVID-19 pandemic: analysis from the North of Italy. Ultrasound Obstet Gynecol. 2020;56(2):289.
doi pubmed - Ahmed AA, Tom BD, Calabrese P. Ectopic pregnancy diagnosis and the pseudo-sac. Fertil Steril. 2004;81(5):1225-1228.
doi pubmed - Ball E, Waters N, Cooper N, Talati C, Mallick R, Rabas S, Mukherjee A, et al. Evidence-Based Guideline on Laparoscopy in Pregnancy: Commissioned by the British Society for Gynaecological Endoscopy (BSGE) Endorsed by the Royal College of Obstetricians & Gynaecologists (RCOG). Facts Views Vis Obgyn. 2019;11(1):5-25.
- RCOG. Guidance for rationalising early pregnancy services in the evolving coronavirus (COVID-19) pandemic, April 2020.
- Alfirevic Z, Farquharson RG. On the 'Diagnostic values of serum hCG on the outcome of pregnancy of unknown location (PUL): a systematic review and meta-analysis'. Hum Reprod Update. 2012;18(6):601-602.
doi pubmed - Wax RS, Christian MD. Practical recommendations for critical care and anesthesiology teams caring for novel coronavirus (2019-nCoV) patients. Can J Anaesth. 2020;67(5):568-576.
doi pubmed - Sehulster L, Chinn RY, Cdc Hicpac. Guidelines for environmental infection control in health-care facilities. Recommendations of CDC and the Healthcare Infection Control Practices Advisory Committee (HICPAC). MMWR Recomm Rep. 2003;52(RR-10):1-42.
- Francis N, Dort J, Cho E, Feldman L, Keller D, Lim R, Mikami D, et al. SAGES and EAES recommendations for minimally invasive surgery during COVID-19 pandemic. Surg Endosc. 2020;34(6):2327-2331.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
