| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website https://www.jcgo.org |
Case Report
Volume 10, Number 1, March 2021, pages 28-32
Isolated Fallopian Tube Torsion: A Rare Cause of Acute Abdomen in Puerperium
Smita Jindala, c, Manisha Mathura, b
aDepartment of Obstetrics and Gynecology, KK Women’s and Children’s Hospital, Singapore
bYong Loo Lin School of Medicine, Duke NUS Medical School, Lee Kong Chian School of Medicine, Singapore
cCorresponding Author: Smita Jindal, Department of Obstetrics and Gynecology, KK Women’s and Children’s Hospital, Singapore
Manuscript submitted November 17, 2020, accepted January 6, 2021, published online March 17, 2021
Short title: Isolated Fallopian Tube Torsion
doi: https://doi.org/10.14740/jcgo706
| Abstract | ▴Top |
Fallopian tube torsion is a type of adnexal torsion and usually occurs in association with an ovarian torsion (termed as tubo-ovarian torsion). Isolated fallopian tube torsion (IFTT) is an extremely rare cause of abdominal pain requiring prompt recognition and treatment. Diagnosis of IFTT during puerperium can be challenging due to the nonspecific nature of clinical features and uncommon objective findings. The management of IFTT is often delayed because of the diagnostic dilemmas. Diagnostic imaging may be suggestive but the diagnosis is often made in retrospect following the surgical intervention. Early recognition and quick intervention are crucial to preserve adnexal function and to minimize morbidity. We describe a case of IFTT in a grand multiparous woman presenting with acute onset right iliac fossa pain and vomiting on the first day postpartum and discuss the difficulties faced in the management of this case along with a review of the literature.
Keywords: Isolated fallopian tube torsion; Abdominal pain; Puerperium
| Introduction | ▴Top |
Isolated fallopian tube torsion (IFTT) is an extremely rare cause of acute abdominal pain in women of reproductive age group and even rarer during pregnancy or puerperium. The incidence of IFFT is approximately one in 1.5 million females [1]. The diagnosis of IFTT as a cause for an acute abdomen during puerperium is often missed or delayed as clinical features and the imaging studies are usually nonspecific. The presentation of IFTT and other puerperium-related disorders associated with an acute abdomen is quite similar. Therefore, the diagnosis is challenging which often delays the definitive treatment of this condition promptly. Surgical management is important in the diagnosis and prognosis of isolated torsion of a fallopian tube and can help to preserve the fertility of the patients desirous of future childbearing [2]. Therefore, special attention should be given to postpartum women with acute abdominal pain when the common causes of a persistent acute abdomen in this age group have been excluded by investigations by having an index of suspicion for the rarer causes such an IFTT.
We report a case of right fallopian tube torsion in the immediate postpartum period which was promptly diagnosed and managed at our institution by a salpingectomy. We also discuss the diagnostic dilemma caused by the rare cause of acute abdomen with a review of the literature.
| Case Report | ▴Top |
Investigations
A 37-year-old, gravida10 para 8 lady, complained of severe and persistent sudden onset acute abdominal pain on the first day postpartum following an uneventful normal vaginal delivery. She had an uneventful antenatal period and had presented in spontaneous labor at term. She underwent a vaginal delivery with an uneventful intrapartum course. She complained of sudden onset sharp right iliac fossa pain associated with nausea and vomiting on the first day postpartum. Her pain score was reported as 8 out of 10. There was no radiation of her pain and she did not report any associated symptoms such as dysuria or frequency of urination, fever, change in bowel habit, or any abnormal vaginal discharge. Her past medical and gynecologic history was noted to be unremarkable, and she had no history of prior episodes of pelvic inflammatory disease or any fertility treatment. Her blood pressure was stable but she had slight tachycardia. On a general assessment, the patient was alert and co-operative but appeared distressed due to pain. On abdominal examination, there was right iliac fossa tenderness and muscle guarding noted on palpation. The uterus was palpable in expectation with her stage of puerperium. On speculum examination, the cervix appeared normal and there was normal appearing lochia discharge in amount and character. A vaginal examination revealed right adnexal tenderness. Her complete blood count showed hemoglobin of 11.5 and total white cell count of 12,000, C-reactive protein (CRP) was 15, serum biochemistry and urinalysis were within normal limits. Endocervical swabs were obtained for culture to exclude an infective cause of the presentation. Renal colic was also considered in initial differential diagnosis but was ruled out by the absence of typical clinical symptoms and a normal abdominopelvic examination. The other differentials that were considered were a pelvic infection, along with other gynecologic emergencies such as hemorrhagic ovarian cyst, ovarian cyst rupture, salpingitis, adnexal torsion, as well as other non-gynecological conditions such as appendicitis.
Diagnosis
The ultrasound pelvis revealed a tubular cystic structure noted in the right adnexa adjacent to the right ovary measuring 4.6 × 3.4 × 4.3 cm. No definite whirlpool sign (twisted vascular pedicle corresponding to the broad ligament, fallopian tube, and adnexal and ovarian branches of the uterine artery or vein) was seen and the right ovary did not show typical signs of torsion (Figs. 1 and 2). Targeted ultrasound of the appendix was performed which was reported to be normal. She was empirically started on intravenous antibiotics and analgesics for her symptoms. However, on account of the persistence of her symptoms, a computed tomographic (CT) imaging for the abdomen and pelvis was performed on day 2 postpartum. The CT examination did not show any evidence of acute appendicitis and was suggestive of the right fallopian tube torsion (Fig. 3).
 Click for large image | Figure 1. Tubular structure adjacent to right adnexa on ultrasound pelvis. |
 Click for large image | Figure 2. Right adnexa on transvaginal ultrasound. |
 Click for large image | Figure 3. Convoluted tubular structure on computed tomography imaging. |
Treatment
Following the CT scan findings, the patient was counseled and consented for a diagnostic laparoscopy to proceed to a salpingectomy or an ovarian cystectomy or a salpingo-oophorectomy. Future fertility was also discussed and the patient expressed to not desire any further pregnancies. She underwent exploratory laparotomy due to technical difficulties encountered with a laparoscopy. Upon a laparotomy, it was noted that there was an adhesion band between the right fallopian tube and the uterus and the right fallopian tube was looped and torted within the adhesion band appearing congested (Fig. 4). The right ovary, the left tube and ovary were normal in appearance. The uterus was approximately 18 weeks in size and otherwise appeared normal. The adhesion band was released and bilateral salpingectomy was performed as the patient was keen for sterilization (Fig. 5).
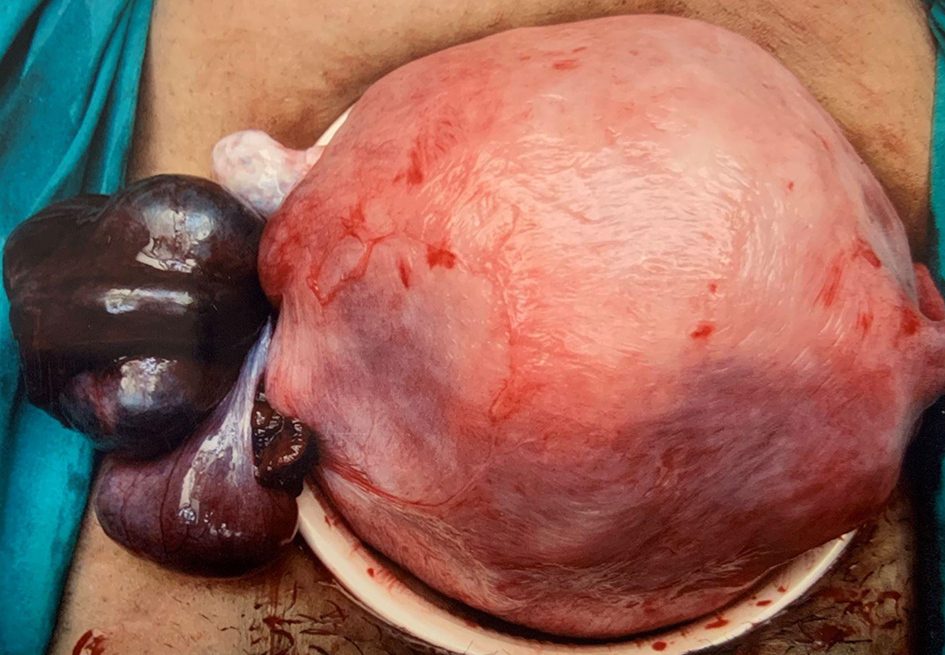 Click for large image | Figure 4. Torted right fallopian tube with the adhesion band. |
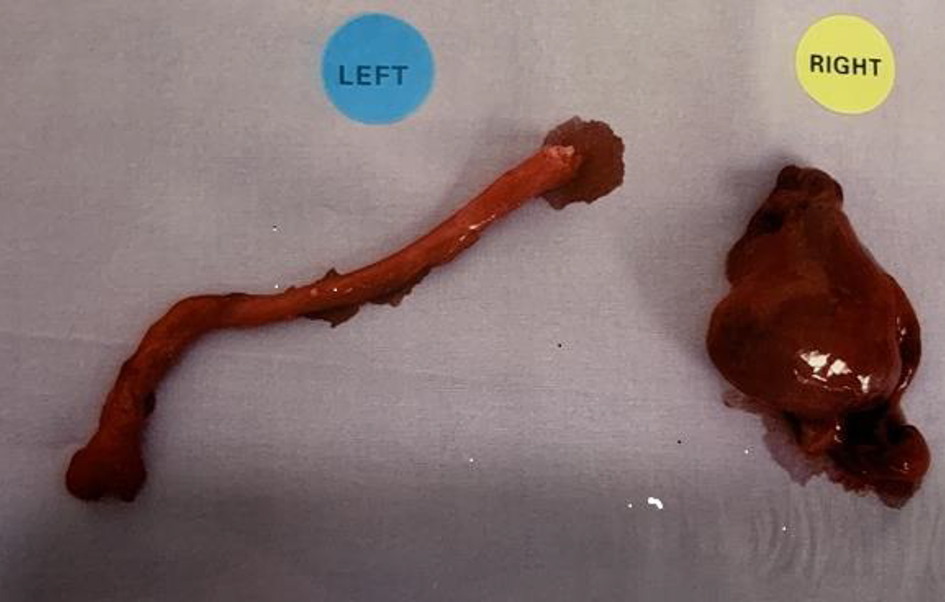 Click for large image | Figure 5. Bilateral fallopian tubes. |
Follow-up and outcomes
The postoperative period was unremarkable and she was discharged well on the third postoperative day. The histopathological examination of the specimen revealed ischemic changes with congestion of the right fallopian tube, consistent with a tubal torsion.
| Discussion | ▴Top |
IFTT is an uncommon cause of lower abdominal pain in women of reproductive age and hence only a few cases of IFTT have been reported in the literature [2-6]. IFTT can pose a diagnostic dilemma due to rarity but more so during the early postpartum period, as the signs and symptoms are nonspecific and can be easily confused with other conditions including adnexal abscess, endometritis, postpartum ovarian vein thrombosis, retroperitoneal hematoma along with non-gynecological causes related to bowel or the urinary system.
The exact mechanism that leads to the isolated torsion of the fallopian tube without the involvement of the ipsilateral ovary is not well understood. Various predisposing factors have been implicated in its occurrence. These include intrinsic factors related to the tubal anatomy and pathophysiology (e.g., pelvic inflammatory disease, tubal pathology like hematosalpinx or hydrosalpinx, tubal tortuosity, paratubal cysts or neoplasm) and extrinsic factors (e.g., adhesions, pelvic congestion, ovarian mass, uterine mass, gravid uterus and drug-related spasms) [7]. Our patient did not have any of these predisposing risk factors.
A review of the literature suggests that the risk of IFTT may increase during pregnancy and that the right fallopian tube is more commonly involved. This may be because of the partial immobilization of the left tube on account of its proximity to the sigmoid mesentery, relatively less venous flow on the right side, and because the clinical presentation of right lower quadrant pain is more often surgically explored due to the suspicion of appendicitis [5-7]. The underlying mechanism of tubal torsion in pregnancy or puerperium is likely caused by a sequential mechanical process, which begins with mechanical blockage of adnexal veins and lymphatic vessels by the gravid uterus. This obstruction can cause pelvic congestion and local edema which results in the enlargement of the fimbrial end, leading to partial to complete torsion of the involved tube [7]. During puerperium, the involution of the uterus causes increased laxity of supporting tissues which can displace the adnexa and increase the predisposition to adnexal torsion. This is most common in the immediate postpartum period [8]. The adnexal torsion in the presented case can be explained by the progressive reduction of the size of the uterus due to the physical involution during the puerperium.
The presenting complaints of the IFTT are sudden onset, severe and sharp lower abdominal pain, associated with nausea, vomiting, fever, or urinary complaints [4, 9]. The physical findings include abdominal tenderness, with or without peritoneal signs, and an inconstant palpable mass [4, 9]. The laboratory findings are usually nonspecific and may show leukocytosis, elevated erythrocyte sedimentation rate (ESR) and CRP.
In the practice of current medicine, imaging is commonly used in the diagnosis of an acute abdomen. In gynecology, ultrasound is often the routine investigation of choice for diagnosis of pelvic pathologies and color Doppler studies have been used to assess ovarian blood supply. The ultrasound findings of IFTT are not pathognomonic and can be non-specific and also quite variable [10]. In women presenting with acute abdominal pain, bowel or urologic causes are usually considered first but their exclusion as a causative agent will often lead to CT scan or magnetic resonance imaging (MRI) as a diagnostic tool.
The diagnostic contribution of ultrasound with Doppler remains controversial in the diagnosis of adnexal torsion [10]. The presence of blood flow on Doppler ultrasonography of the adnexa has a poor negative predictive value. In a study by Pena et al, 60% of the surgically confirmed cases of torsion had a normal Doppler flow, hence suggesting that normal blood flow cannot exclude a torsion [11]. The ultrasound features in IFTT usually constitute a normal-appearing uterus and ovaries with normal flow, physiological free fluid, a dilated tube with thickened, echogenic walls, or a convoluted echogenic mass thought to represent a thickened and torted fallopian tube [12].
Hiller et al reported that the correct preoperative diagnosis of adnexal torsion based on CT findings was made in only 34% of patients suggesting that the diagnostic accuracy of adnexal torsion based on CT findings seems to be low [13]. An MRI can be a valuable tool in recognizing adnexal torsion due to its sensitivity in detailing soft tissue masses. The CT and MRI features of adnexal torsion or IFTT usually include fallopian tube thickening, smooth wall thickening of the twisted adnexal cystic mass, dilated tube greater than 15 mm, or luminal CT attenuation greater than 50 Hounsfield Unit. Secondary features can include ascites, peritubular fat stranding, thickening, and/or enhancement of broad ligament and uterine deviation to the twisted side [14, 15].
Thus, despite advancement in diagnostic accuracy with current day available imaging modalities, an accurate diagnosis of acute abdomen is often established in retrospect following the surgical intervention in certain conditions such as an IFTT. A diagnostic or a therapeutic laparoscopy is the most specific diagnostic tool for evaluating adnexal torsion/IFTT and treating this condition inpatient suitable for a laparoscopy. Early surgical intervention is recommended for women of reproductive age group presenting with persistent acute abdominal pain after the exclusion of infective causes to reduce morbidity and to maximize the chance of preserving her fertility. Necrosis of fallopian tube can also lead to irreversible damage of ipsilateral ovary [15]. A torted adnexal mass undergoing necrosis has the potential to cause serious infection similar to that of perforated appendicitis in case of delayed intervention [16]. Additionally, early intervention can sometimes salvage torted tissue by detorsion if it is performed on time [17].
In this case, laparotomy was performed given the enlarged uterine size in the immediate postpartum state of the patient and the experience of the operating team which appears essential in the decision making as to the route of surgery. A salpingectomy was recommended in this case for the gangrenous fallopian tube as a result of torsion. The patient underwent a laparotomy and bilateral salpingectomy, because of the gangrenous right fallopian tube and her desire for permanent sterilization as she had completed her family. The postoperative period was uneventful, and the patient was discharged well on the third postoperative day.
Conclusion
IFTT is an extremely rare cause of acute abdomen in women of reproductive age group, more so during puerperium or pregnancy. The diagnosis of IFTT requires a high index of suspicion due to its nonspecific presentation and its rarity but it should be considered as a differential diagnosis of acute pelvic pain following the exclusion of the common causes of a persistent acute abdomen in this age group. Imaging techniques can be suggestive but might not be conclusive in formulating a diagnosis and hence surgical management remains the gold standard for its definitive diagnosis and management. An early diagnosis and timely intervention is important to reduce morbidity and preserve fertility in women desirous of future fertility.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Informed consent was taken from the patient.
Author Contributions
Jindal wrote the manuscript with the guidance of Mathur. Both Jindal and Mathur were directly involved in the care of the patient described in the case report.
Data Availability
The authors declare that data supporting the findings of this case report are available within the article.
| References | ▴Top |
- Hansen OH. Isolated torsion of the Fallopian tube. Acta Obstet Gynecol Scand. 1970;49(1):3-6.
doi pubmed - Sun Y, Liu LL, Di JM. Isolated tubal torsion in the third trimester of pregnancy: A case report and review of the literature. J Res Med Sci. 2014;19(11):1106-1109.
- Batukan C, Ozgun MT, Turkyilmaz C, Tayyar M. Isolated torsion of the fallopian tube during pregnancy: a case report. J Reprod Med. 2007;52(8):745-747.
- Origoni M, Cavoretto P, Conti E, Ferrari A. Isolated tubal torsion in pregnancy. Eur J Obstet Gynecol Reprod Biol. 2009;146(2):116-120.
doi pubmed - Phupong V, Intharasakda P. Twisted fallopian tube in pregnancy: a case report. BMC Pregnancy Childbirth. 2001;1(1):5.
doi pubmed - Yalcin OT, Hassa H, Zeytinoglu S, Isiksoy S. Isolated torsion of fallopian tube during pregnancy; report of two cases. Eur J Obstet Gynecol Reprod Biol. 1997;74(2):179-182.
doi - Bernardus RE, Van der Slikke JW, Roex AJ, Dijkhuizen GH, Stolk JG. Torsion of the fallopian tube: some considerations on its etiology. Obstet Gynecol. 1984;64(5):675-678.
- Cappell MS, Friedel D. Abdominal pain during pregnancy. Gastroenterol Clin North Am. 2003;32(1):1-58.
doi - Krissi H, Shalev J, Bar-Hava I, Langer R, Herman A, Kaplan B. Fallopian tube torsion: laparoscopic evaluation and treatment of a rare gynecological entity. J Am Board Fam Pract. 2001;14(4):274-277.
- Chang HC, Bhatt S, Dogra VS. Pearls and pitfalls in diagnosis of ovarian torsion. Radiographics. 2008;28(5):1355-1368.
doi pubmed - Pena JE, Ufberg D, Cooney N, Denis AL. Usefulness of Doppler sonography in the diagnosis of ovarian torsion. Fertil Steril. 2000;73(5):1047-1050.
doi - Gross M, Blumstein SL, Chow LC. Isolated fallopian tube torsion: a rare twist on a common theme. AJR Am J Roentgenol. 2005;185(6):1590-1592.
doi pubmed - Hiller N, Appelbaum L, Simanovsky N, Lev-Sagi A, Aharoni D, Sella T. CT features of adnexal torsion. AJR Am J Roentgenol. 2007;189(1):124-129.
doi pubmed - Rha SE, Byun JY, Jung SE, Jung JI, Choi BG, Kim BS, Kim H, et al. CT and MR imaging features of adnexal torsion. Radiographics. 2002;22(2):283-294.
doi pubmed - Ghossain MA, Buy JN, Bazot M, Haddad S, Guinet C, Malbec L, Hugol D, et al. CT in adnexal torsion with emphasis on tubal findings: correlation with US. J Comput Assist Tomogr. 1994;18(4):619-625.
doi pubmed - Ferrera PC, Kass LE, Verdile VP. Torsion of the fallopian tube. Am J Emerg Med. 1995;13(3):312-314.
doi - Taskin O, Birincioglu M, Aydin A, Buhur A, Burak F, Yilmaz I, Wheeler JM. The effects of twisted ischaemic adnexa managed by detorsion on ovarian viability and histology: an ischaemia-reperfusion rodent model. Hum Reprod. 1998;13(1O):2823-2827.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
