| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website https://www.jcgo.org |
Case Report
Volume 11, Number 4, December 2022, pages 108-112
Will the Scan Change the Plan? Point of Care Ultrasound for Timely Decision Making in a Rural Obstetrics and Gynecology Department
Scott Taylora, b, Kelly Nga, Brian McCullya
aDepartment of Obstetrics and Gynaecology, Mildura Base Public Hospital, Mildura, Australia
bCorresponding Author: Scott Taylor, Department of Obstetrics and Gynaecology, Mildura Base Public Hospital, Mildura, Australia
Manuscript submitted July 19, 2022, accepted October 22, 2022, published online December 30, 2022
Short title: Ultrasound in Obstetrics and Gynecology Department
doi: https://doi.org/10.14740/jcgo816
| Abstract | ▴Top |
In rural and remote hospitals, access to urgent ultrasound especially out-of-hours can pose a barrier to timely clinical decision making. Focused Assessment with Sonography for Trauma (FAST) is a common practice in emergency departments to quickly identify abnormal free fluid in trauma patients and can allow targeted, early intervention. Where intraabdominal free fluid is present in the non-trauma population, a similar technique to FAST scanning called Focused Assessment for Free Fluid (FAFF) can be a simple and time-saving tool to facilitate and escalate emergency management. A ruptured ectopic pregnancy is a common gynecology emergency that may be associated with significant intraabdominal bleeding. This bleeding may be seen on FAFF as free fluid in the pelvis or upper abdomen allowing early decision making including surgical intervention, especially where there may be a delay in attaining formal sonographic assessment. In this case report, we describe the management of ectopic pregnancy presenting in a rural emergency department where FAFF ultrasound provided the diagnostic confidence to proceed to theater when access to formal sonography was delayed.
Keywords: Ectopic pregnancy; FAFF scan; Point of care ultrasound; Intraabdominal free fluid
| Introduction | ▴Top |
Ectopic pregnancy is a relatively common, acute gynecological presentation to the emergency department. It may complicate 1-2% of all early pregnancies, and is one of the leading causes of morbidity and death for women in the first trimester [1]. Trans-vaginal ultrasound is widely considered the best diagnostic tool for identifying an ectopic pregnancy, particularly when patients present without evidence of significant hemodynamic compromise [2]. In rural and remote settings, access to urgent ultrasound may be limited. In contrast, nearly all emergency departments have point of care (portable or bedside) ultrasound machines on-site. Additionally, emergency doctors are often trained in Focused Assessment with Sonography for Trauma (FAST) scans to identify free fluid in the abdomen, pelvis and thorax to enable rapid intervention when required [3]. There is now increasing evidence that this may also benefit non-trauma patients, where free fluid can herald signs of abnormal bleeding such as may be present with an ectopic pregnancy, and thus minimize delay for definitive surgical care [3, 4]. This is referred to as Focused Assessment for Free Fluid (FAFF) scanning (Figs. 1-3) in the current literature and is essentially synonymous with FAST scanning [3, 5]. In developed countries such as Australia, death or serious morbidity consequent to ectopic pregnancy is fortuitously rare. Notwithstanding this, delay to definitive management which may include laparoscopy, is a significant contributor to escalation of harm [2]. The following case report describes the use of bedside ultrasound for assessment of free fluid as a clinical decision making tool when access to formal scanning was limited. As a result, the time taken to action successful surgical management was minimized and the patient had a safe and uncomplicated recovery.
 Click for large image | Figure 1. Focused assessment of fluid in the right upper quadrant. |
 Click for large image | Figure 2. Focused assessment of fluid in the left upper quadrant. |
 Click for large image | Figure 3. Focused assessment of free fluid in the lower abdomen. |
| Case Report | ▴Top |
Investigations
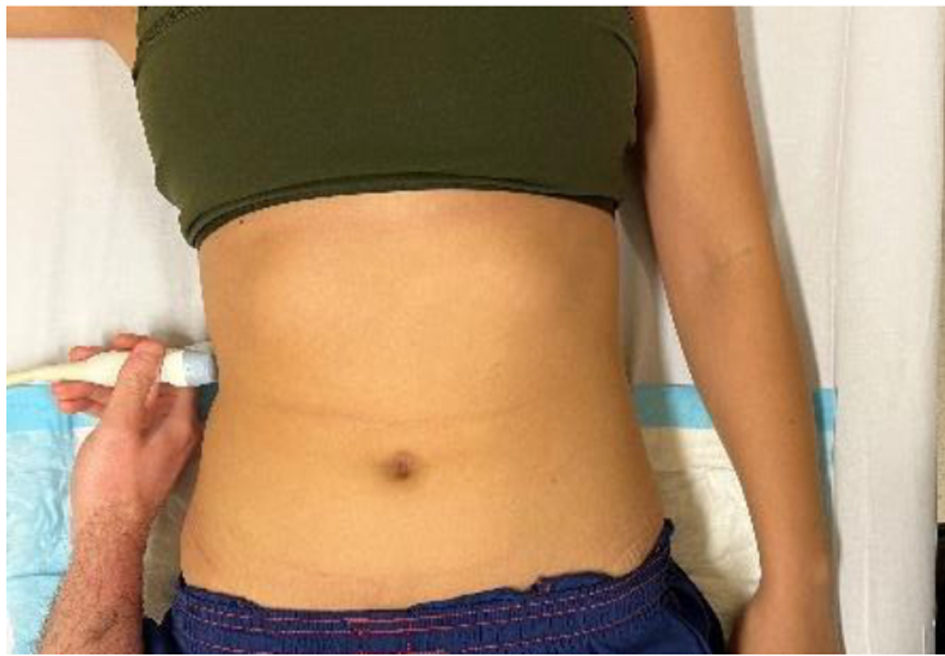
A gravida 1, 30-year-old woman presented to the emergency department late in the evening with a 1-day history of vaginal spotting and intermittent lower abdominal cramping with pain radiating to the right shoulder tip. She was approximately 4 weeks pregnant by last menstrual period and had been well prior to the onset of symptoms. On arrival, she was mildly tachycardic with a heart rate (HR) of 107 beats per minute, but hemodynamically stable with a blood pressure (BP) of 118/92 mm Hg with no postural drop. Her respiration rate (RR) was 20 breaths per minute, with oxygen saturation (SpO2) of 100% on room air. She was afebrile. Her admission urine beta-human chorionic gonadotropin (beta-hCG) was positive.
She was seen by the emergency physician approximately 3 h later and her vital signs remained unchanged. On examination, she had mild suprapubic and right lower abdominal tenderness without rebound tenderness, rigidity or distension. Her cervix was closed and no active bleeding was noted on speculum examination. Her hemoglobin was 128 g/L, white cell count was 18.4 × 109/L, and C-reactive protein was 4 mg/L. Her quantitative beta-hCG was 316 mIU/mL. The clinical impression was that of a threatened miscarriage and the patient was kept for observation pending review by the gynecology on-call team which occurred shortly after midnight. In the interlude, there were no changes of clinical status, and importantly, no evidence of deterioration. After review from the night obstetrics and gynecology registrar, the situation was appropriately acknowledged to be a pregnancy of unknown location, and warranted urgent ultrasound to assist diagnosis. However, given her vitals remained stable and the pain was manageable, it was deemed that she did not meet criteria for on-call sonography and arrangements were therefore made to schedule examination for the start of the following working day.
Diagnosis
The patient remained in the emergency department overnight. She remained symptomatic as per initial presentation. Her observations were stable with HR of 88 beats per minute, BP of 112/70 mm Hg, RR of 18 breaths per minute, SpO2 of 100%, and temperature of 36.7 °C. A repeat hemoglobin at 07:40 was 106 g/L. A bedside FAFF ultrasound was performed by the on-coming gynecology team. Free fluid was identified in the right upper quadrant in Morison’s pouch (Fig. 4) as well as in the left upper quadrant. Fluid and adnexal debris was also noted adjacent to the bladder. There was no evidence of an intrauterine pregnancy. In view of the likely diagnosis of ruptured ectopic pregnancy, given the free fluid, no intrauterine pregnancy, and falling hemoglobin, the decision was made to cancel the formal transvaginal ultrasound which was yet to be performed, and to transfer the patient immediately to the operating suite for a diagnostic laparoscopy.
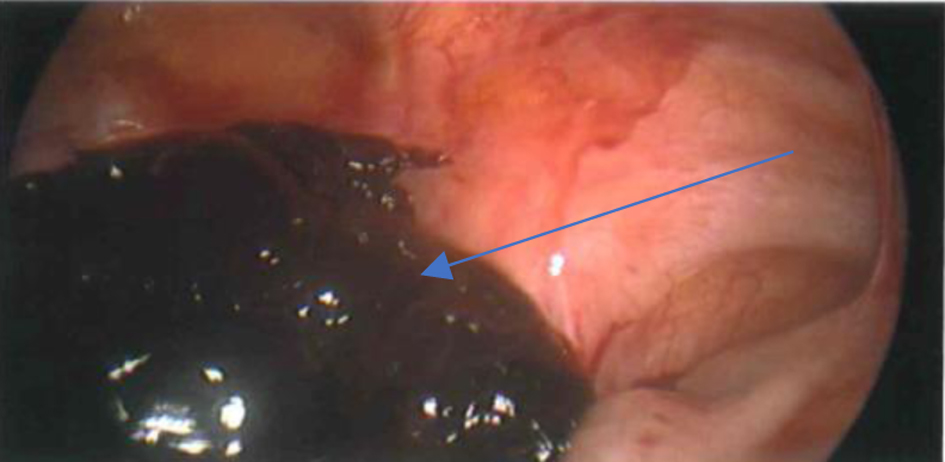 Click for large image | Figure 4. Hemoperitoneum. |
Treatment
Laparoscopy demonstrated significant intraabdominal blood clot with estimated volume of 1,200 mL. A right, unruptured ampullary ectopic pregnancy was identified with active bleeding noted from the fimbria and ostia (Figs. 4 and 5). An attempt to conserve the tube by extracting visible clot and sac from the lumen was unsuccessful. A salpingectomy was then performed with resolution of bleeding and restoration of anatomy. Both ovaries were normal as was the remaining left tube. Prior to closure, the pelvis and abdomen were irrigated and all visible clot removed. There was no evidence of other pelvic disease.
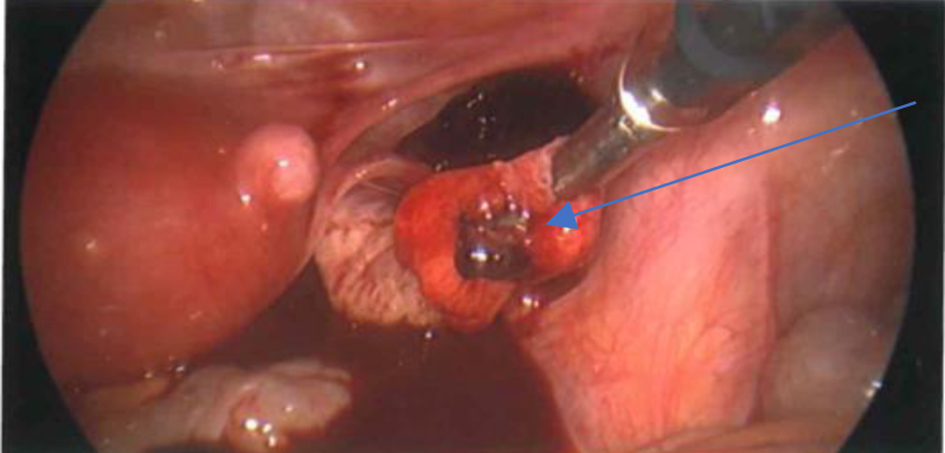 Click for large image | Figure 5. Right tubal ectopic pregnancy. |
Follow-up and outcomes
The patient recovered well post-operatively. Her hemoglobin was 86 g/L, and she did not require transfusion. She was discharged the following day on oral iron supplementation. Histopathology confirmed tubal ectopic pregnancy. She had an uneventful recovery and was well when reviewed in the outpatient clinic 6 weeks later.
| Discussion | ▴Top |
The case demonstrates the importance of prompt clinical diagnosis, particularly rural settings where an evolving complication must be recognized quickly to allow appropriate intervention. We acknowledge however that this does not always occur. We note that the patient presented with a known early pregnancy, vaginal bleeding and abdominal discomfort associated most significantly, with shoulder-tip pain. This is almost always pathopneumonic of diaphragmatic irritation secondary to intraabdominal bleeding and as such, would normally raise suspicion of a likely ruptured ectopic pregnancy. That it did not, is not a point of blame, but rather an opportunity to learn from what is now known, as indeed is the aim of all case reviews such as this.
We also recognize the impediments of rural hospital practice. Whilst in this case, the history and clinical findings alone may well have been sufficient to dictate management, there are many instances where the use of ancillary ultrasound is vital for diagnostic certainty or for the rationalization of an appropriate clinical strategy. Unfortunately, it is not always possible to do so, or to access the skill of trained operators to support this service on an “around the clock” basis. Because of this, procedures are often bulked together for daylight hours when expertise is more readily available. This is an entirely practical solution, but requires effective triage principals to minimize the risk of inappropriate delay or failed prioritization of actual clinical urgency. In answer to this, our case demonstrates the effectiveness of point of care ultrasound to reduce the reliance upon ancillary procedures and yet with equal efficacy, to target diagnostic acumen to critically assist urgent decision making. This is because FAFF can be used to quickly and reliably identify free fluid in the abdomen or pelvis as well as the chest and pericardium. In the setting of trauma or suspected pathology such as an ectopic pregnancy, this finding may well be enough to confirm the suspicion of abnormal bleeding in a patient who may or may not be symptomatic. In the former, the diagnosis may be critical to expedite urgent resuscitative care; in the latter, it can be equally vital to identify the risk of imminent compromise prior to the declaration of clinical signs or catastrophic deterioration. In our case, the positive FAFF scan was sufficient to confirm the suspicion of intraabdominal bleeding and to circumvent any further delay encumbering immediate operative care.
In our case, the patient’s cardiovascular findings had remained stable up to this time. Advanced Trauma Life Support (ATLS) cautions that blood loss up to 750 mL or 15% of circulating blood volume may be associated with normal vital signs [6]. Similarly, loss of up to 1,500 mL or 30% total blood volume may yield only slight aberrations of HR, RR, and BP findings [6]. This means that diagnosis, or more importantly, rapid diagnosis in the setting of an evolving hemorrhagic process may be delayed if waiting for abnormal observations, leading to the risk of sudden, circulatory collapse. To confound matters, the utility of serial hemoglobin estimations may be falsely reassuring, for whilst a sudden or measurable drop may be indicative of blood loss, there are little reported data to demonstrate just how closely this reflects actual hemoglobin depletion. In contrast, FAFF ultrasound can detect intraabdominal hemorrhage as little as 200 - 250 mL, which may be long before clinical signs have had time to evolve [7]. It may also be used to quantitate higher volumes by determining where the fluid has tracked or pooled. Intraabdominal bleeding tends first to accumulate in the pelvis, particularly in the pouch of Douglas which is the lower most point of the pelvis when standing and lying supine. With more substantial bleeding, the fluid can be visualized in Morison’s pouch which is the space between the right kidney and liver (Fig. 6) [8]. This usually equates to a hemorrhage of at least 650 mL of blood [7]. When it is found additionally in the left upper quadrant adjacent to the spleen, the loss may be greater still. FAFF is therefore a valuable diagnostic tool for the identification of abnormal free fluid, and for the estimation of blood loss that that fluid most likely represents. But there are some caveats to this interpretation. The procedure can identify free fluid, and when this occurs in areas where fluid is not meant to be or is in a volume that is greater than would normally be expected, it is very likely to be abnormal. What that fluid is however, cannot be ascertained without direct observation. In our case, as indeed in cases of trauma, the etiology of injury is such that it is most likely to be blood but there may be other instances where it could just as easily be an inflammatory collection or exudate or the contents encapsulated within the walls of an unexpected cyst. In a recent article, we cited the rare finding of a large dermoid cyst misdiagnosed as free intraabdominal fluid in a patient presenting with presumed ectopic pregnancy [9]. In this case, the findings were documented by conventional ultrasound examination. FAFF scanning was not performed but had it been done, we questioned whether examination of the upper quadrants would have demonstrated extension of that fluid into the upper quadrants. We suspect that it would not. In this case, the patient was taken for immediate emergency surgery where, not surprisingly, no bleeding was identified [9]. The case puts emphasis on a combined role of FAFF and conventional scanning techniques to ascertain the significance of abnormal free fluid when found in isolation by the latter.
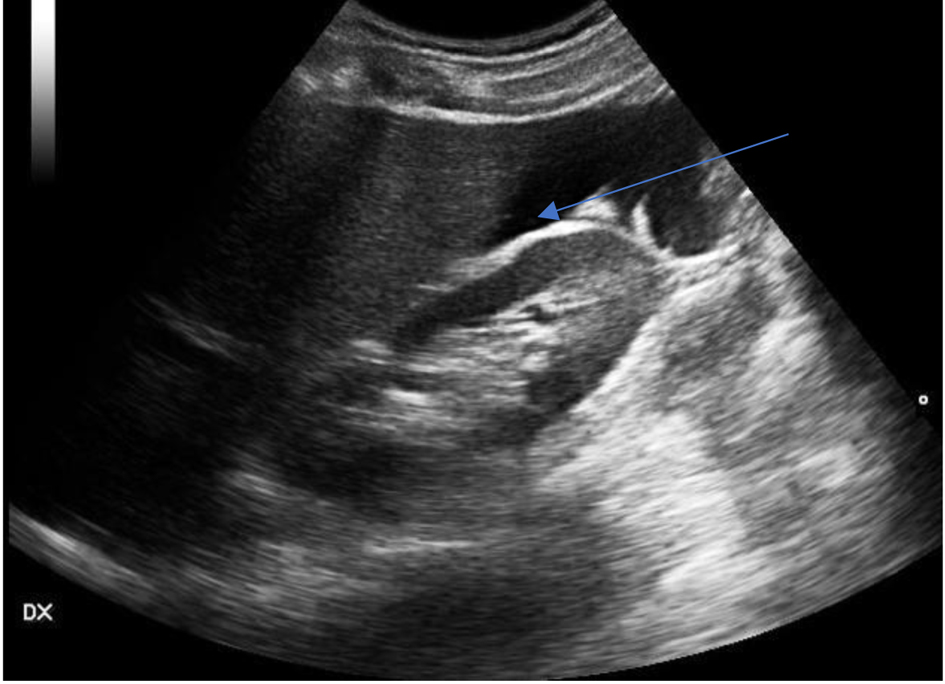 Click for large image | Figure 6. Free fluid located in Morison’s pouch between the liver and kidney [8]. |
The ability to perform FASS scanning competently is a skill easily acquired by all medical and nursing staff. Evidence affirms that when they do so, they are at least as good as radiologists at detecting abnormal free fluid [3]. There is therefore an opportunity to empower an almost unlimited capacity to effectively utilize this diagnostic tool in acute, primary care environments. The impact of having competent providers trained in point of care ultrasound is no more so evident than in rural hospital settings where access to formal ultrasound services is limited or fiercely bartered, or is otherwise constrained by working hours. It means ultimately, that patient safety is championed no matter where that patient is treated. By incorporating FAFF scanning in acute care and evaluation, management decisions can be immediate, appropriate and based on best available evidence of risk. Our case demonstrates one such example. None of the procedures undertaken were extraordinary or unusual, and they were just simply part of normal comprehensive care supported by the procedures described. We present this case not to highlight ourselves, but to highlight the ease with which these techniques can be used.
Learning points
Intraabdominal hemorrhage may be clinically significant prior to hemodynamic compromise, particularly in young healthy patients.
FAFF, using ultrasound to determine if abdominal free fluid is present, can detect intraabdominal hemorrhage well before hemodynamic compromise occurs.
FAFF scanning is a skill that can be easily taught, and is useful in a number of specialties including emergency and obstetrics and gynecology.
FAFF scans may help to aid clinical decision making, particularly in rural settings where access to formal scans can be limited by time of day or availability of trained sonographers.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Informed consent was obtained from the patient.
Author Contributions
The primary author wrote the introduction and discussion, and was the primary surgeon on the case. The secondary author wrote the case report and the abstract and was the admitting doctor. The third author was the supervisor, who edited the report, and who was present at the operation.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
| References | ▴Top |
- Adhikari S, Blaivas M, Lyon M. Diagnosis and management of ectopic pregnancy using bedside transvaginal ultrasonography in the ED: a 2-year experience. Am J Emerg Med. 2007;25(6):591-596.
doi pubmed - Sivalingam V, Duncan C, Kirk E, Shephard L, Horne A. Diagnosis and management of ctopic pregnancy. J Fam Plann Reprod Health Care. 2011;37:231-240.
doi pubmed - Maitra S, Jarman R, Halford N, Richards S. When FAST is a FAFF: is FAST scanning useful in non-trauma patients? Ultrasound. 2008;16(3):165-168.
doi - Dart R, McLean S, Dart L. Isolated fluid in the Cul-de-Sac: how well does it predict ectopic pregnancy? American Journal of Emergency Medicine. 2002;20(1):1-4.
doi pubmed - Baston C, Moore C, Krebs EA, Dean A, Panebianco N. Pocket guide to POCUS: point-of-care tips for point-of-care ultrasound. McGraw Hill; 2018. Available from: https://accessmedicine.mhmedical.com/content.aspx?bookid=2544§ionid=210277485.
- Nickson C. Major Haemorrhage in Trauma. 2020. Accessed on May 26, 2022.
- Pariyadath M, Snead G. Emergency ultrasound in adults with abdominal and thoracic trauma. 2021. Available from: https://www.uptodate.com/contents/emergency-ultrasound-in-adults-with-abdominal-and-thoracic-trauma?search=FAST%20scans&source=search_result&selectedTitle=1∼150&usage_type=default&display_rank=1.
- Bickle I, Botz B. Focussed assessment with sonography for trauma (FAST) scan. Reference article, Radiopaedia.org. Accessed on Jul 7, 2022.
doi - Aboda A, McCully B. Cognitive conflict - how to deal with sudden, unsuspected shifts of the treatment paradigm. Juniper Online Journal of Case Studies. 2022;13(4):555861.
doi
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
