| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website https://www.jcgo.org |
Case Report
Volume 12, Number 1, March 2023, pages 15-18
Rh-Isoimmunization in a Primigravida Skydiver
Hector O. Chapaa, c, Carley Hagarb, Armand Tadjalib, Elias Perlib
aDepartment of Obstetrics and Gynecology, Texas A&M University School of Medicine, College Station, TX, USA
bTexas A&M University School of Medicine, College Station, TX, USA
cCorresponding Author: Hector O. Chapa, Department of Obstetrics and Gynecology, Texas A&M University School of Medicine, College Station, TX, USA
Manuscript submitted November 23, 2022, accepted January 6, 2023, published online March 21, 2023
Short title: Rh-Isoimmunization in a Primigravida Skydiver
doi: https://doi.org/10.14740/jcgo845
| Abstract | ▴Top |
There is a paucity of data on risks of skydiving while pregnant. Although the American College of Obstetricians and Gynecologists states to avoid the activity in pregnancy, women may underestimate potential complications from it and may continue to skydive while pregnant or may do so inadvertently if unaware of their pregnancy. We present a unique case of a primigravida who completed 100 jumps at 10,000 feet throughout her gestation, as she was unaware of her pregnant state, associated with Rh-isoimmunization presumably from chronic placental abruption. A 20-year-old Caucasian female presented to an urgent care center for abdominal cramping thought to be secondary to constipation. A urine pregnancy test was performed due to irregular menstruation history. Although the patient denied being pregnant, urine chorionic gonadotrophic hormone testing was positive with physical examination suggesting 32 - 34 weeks of gestation. The patient was a professional skydiving photographer with 100 logged jumps from the start of her pregnancy (by estimated gestational age calculation). She stated irregular vaginal bleeding every 4 - 6 weeks throughout the time of pregnancy, which she interpreted as her menstruation. Her abdominal discomforts were diagnosed as active labor, and she progressed to preterm delivery at 34 weeks (gestational age assigned to the newborn at delivery based on neonatal assessment). Port-wine-stained amniotic fluid was noted at the time of spontaneous membrane rupture suspicious for chronic abruption. The patient was Rh negative and found to possess anti-D antibody, confirming Rh sensitization. Placental histology revealed a placental mass of 438 g, retroplacental adherent fibrin deposition with placental parenchymal compression. A 40% parenchymal infarct was present. Skydiving while pregnant poses several risks to the maternal-fetal unit. Rapid deceleration from parachute canopy deployment and/or repeated impact from landing(s) may lead to placental abruption (acute or chronic). This can result in Rh-isoimmunization in the susceptible patient, and preterm birth. In cases of massive or repeated abruption events, fetal death may be a potential outcome. Beyond the rarity and novel nature of habitual skydiving while pregnant, this case underscores the need for increased access to contraceptive agents, especially for those persons with physical risk-taking behaviors.
Keywords: Primigravida; Rh-isoimmunization; Rh sensitization; Skydiving; Fetal-maternal hemorrhage; Preterm birth
| Introduction | ▴Top |
The actual effects/risks of skydiving while pregnant is not known but may include hypoxia from low oxygen saturation at high altitudes, mechanical forces during canopy opening or landing, and extremity fractures from ground impact [1]. In worst cases, a fatality may occur, usually from landing errors or fast canopies/intentional fast landing [2]. We present a rare case of suspected chronic placental abruption with associated Rh-isoimmunization occurring in a primigravida who logged 100 skydives while unaware of her pregnancy, culminating in preterm birth at 32 weeks.
| Case Report | ▴Top |
A 20-year-old Caucasian female presented to an urgent care center for abdominal cramping thought to be secondary to constipation (Fig. 1). Medical, family, and psychosocial history are non-contributory. She reported irregular monthly vaginal bleeding with an unsure last menstrual period. The patient was a professional skydiving photographer with 100 logged jumps from the start of her pregnancy (by estimated gestational age calculation) (Fig. 1). Although the patient was seen by her gynecologist 1 year prior, effective contraception was not addressed at that time. At the urgent care center, a urine pregnancy test was collected; it was positive. The patient, a primigravida, was unaware of her pregnancy. Fundal height on physical examination was 32 - 34 weeks, and fetal cardiac activity was confirmed by handheld Doppler device. Her cervical examination was 2 cm dilation, 90% effacement, 0 station with an intact amniotic sac. She was transferred to our hospital for pregnancy evaluation and labor assessment. Upon arrival to the maternity unit, she was found to be 6cm dilated, 100% effaced, and +1 station (Fig. 1). Bedside ultrasound provided an estimated gestational age of 32 weeks, with normal amniotic fluid. The fetus was in a cephalic presentation. Spontaneous amniorrhexis occurred immediately prior to fetal delivery, revealing port-wine-stained fluid. The patient quickly progressed to a spontaneous vaginal birth of a viable male with birthweight 2,340 g and Apgar’s of 7 (1 min) and 9 (5 min). The patient was not a smoker, was non-hypertensive, and a urine screen for illicit drugs was negative.
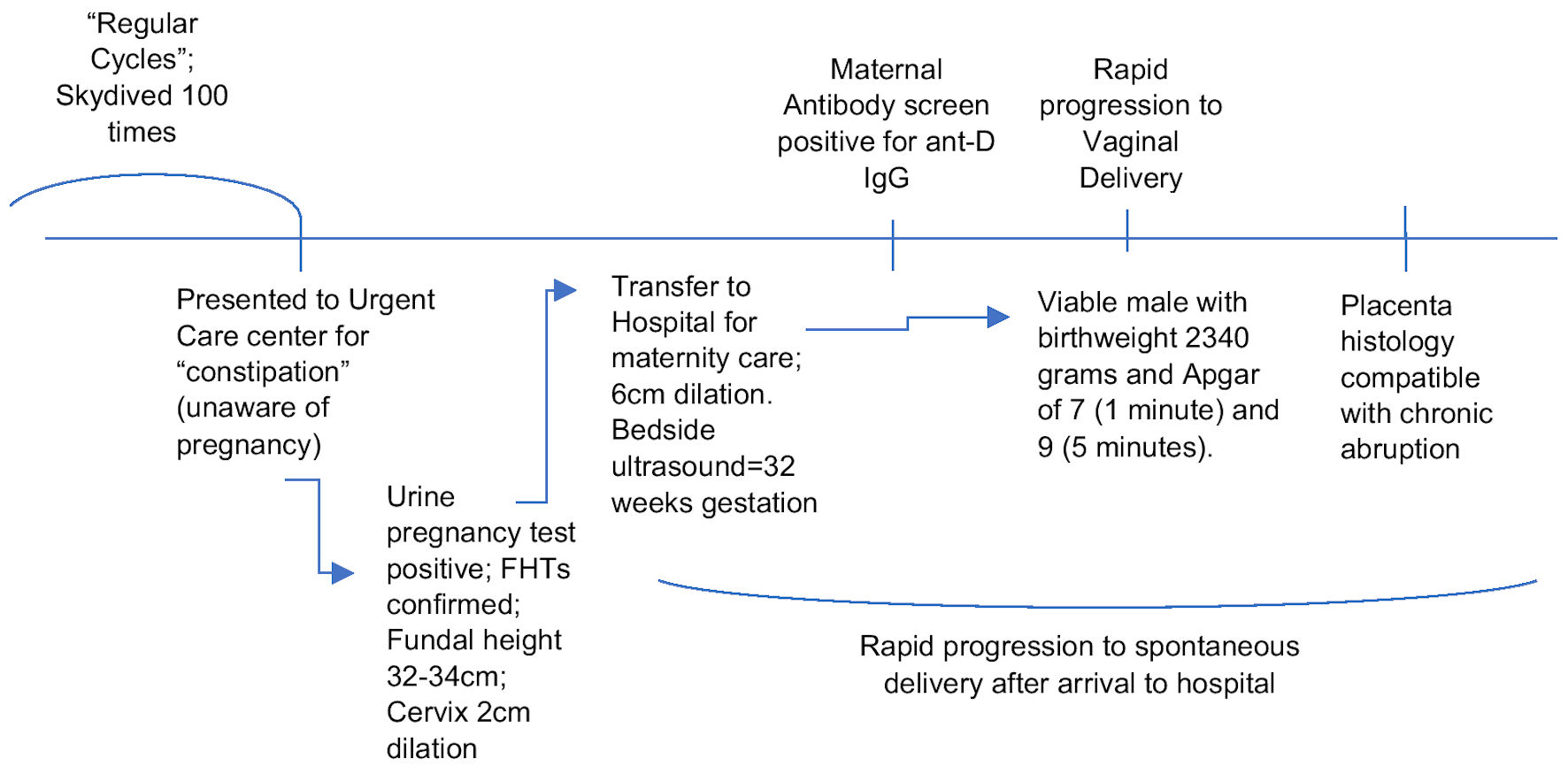 Click for large image | Figure 1. Patient’s history and obstetrical care timeline. FHTs: fetal heart tones; Ig: immunoglobulin. |
Umbilical arterial cord gas revealed a pH of 7.27 and base excess of -4. The patient’s blood type was O, Rh negative. Anti-D antibody was detected in the maternal serum at a titer of 1:16 (Fig. 1). The patient’s fibrinogen was normal, and her admission hematocrit was 28%. Maternal serum Kleihauer-Betke (KB) test was negative for fetal cells. Placental histology revealed a placental mass of 438 g, retroplacental adherent fibrin deposition with placental parenchymal compression. A 40% parenchymal infarct was present. We acknowledge that this patient may have become Rh sensitized by other factors as well, including the gestational age of the pregnancy. However, the patient’s 100 logged skydives is the most impactful clinical risk factor for isoimmunization. The patient’s clinical history of episodic vaginal bleeding throughout her gestation, identification of port-wine-stained amniotic fluid, presenting preterm labor and delivery, and the placental histology support a clinical diagnosis of chronic abruption (Fig. 1).
A dose of betamethasone was administered intramuscularly for fetal lung maturity augmentation, and intravenous magnesium sulfate was begun for fetal neuroprotection upon the patient’s transfer to the maternity unit.
The patient repeatedly verbalized to hospital staff that she was unaware of her pregnancy status. Although initially shocked by the pregnancy diagnosis and labor process, she expressed happiness and relief that the child was healthy and stable. Social work (case management) was involved in the postpartum care and discharge planning. The mother-child pair was discharged home without incident on the second postpartum day. The importance of future, early prenatal care due to her Rh-isoimmunization status was communicated to the patient on multiple occasions. She declined initiation of contraception at the time of hospital discharge.
| Discussion | ▴Top |
This case report is the first to describe Rh-isoimmunization in a primigravida likely associated with repeated skydiving (more than 100 documented jumps) while pregnant. The American College of Obstetricians and Gynecologists (ACOG) lists skydiving as an activity to avoid while pregnant [3]. Not unexpectedly, the medical literature is void of publications in this area. We conducted a literature search using the terms “skydive”, “parachute”, and “skydive and pregnancy” and found only one publication. This 2014 publication was an international retrospective anonymous online questionnaire on skydivers’ epidemiology, experience, and pregnancy-related information [1]. This online link was sent out to the International Parachuting Commission (FAI/IPC) and national parachuting federations directly. Additionally, the study was posted in online discussion forums on skydiving and pregnancy. Fifty-seven parous female skydivers responded and completed the questionnaire, between September and November 2010. The questionnaire was answered from world-wide IP addresses. The survey results showed that the majority of skydivers continued the activity while pregnant, and did try to reduce the risk of injuries as much as possible (restricted skydiving activity to “blue skies” (n = 14), use of “slower parachutes” (n = 9), “taking it easier” (n = 6), employing “special aircraft exit” (n = 1), use of additional “special packing” (n = 1) or “team jumps only” (n = 1), and/or jumping under “no wind” conditions (n = 7)). This indicates an active decision to continue skydiving during pregnancy, despite the potential risks and the lack of research in this area. Eight participants described pregnancy-related problems: three had hypertension, two diabetes, one preterm labor, one preeclampsia, and one placenta previa. Although the authors included a question on pregnancy complications, no details of adverse pregnancy outcomes or information on the child’s development was ascertained, due to possible participation bias with that reporting.
The actual risks of skydiving while pregnant are not known. However, potential sources of maternal morbidity include low oxygen saturation at high altitudes, mechanical forces during canopy opening or landing, and extremity fractures from ground impact [1]. According to Parks College Parachute Research Group, canopy opening shock forces range from between 3 and 6 g (gravity unit) and have also documented hard openings of 9 to 12 g [4]. As described by Ebner et al, a motor vehicle accident at 30 km/h into a concrete wall with a 50-cm crumple zone decelerates at 7 g [1]. These forces are more than capable of resulting in placental abruption due to force transmission to the uterus.
We acknowledge that this patient may have become Rh sensitized by other factors as well, including the gestational age of the pregnancy. However, the patient’s 100 logged skydives is the most impactful clinical risk factor for isoimmunization. The patient’s clinical history of episodic vaginal bleeding throughout her gestation, identification of port-wine-stained amniotic fluid, presenting preterm labor and delivery, and the placental histology support a clinical diagnosis of chronic abruption. Although the anti-D antibody titer was found to be 1:16, we cannot speculate whether that was peak titer or not, or when the actual sensitization first occurred. The patient’s KB test was negative for fetal cells. The patient’s KB test was negative. This favors our clinical deductions that this was a chronic process rather than an acute fetal-maternal hemorrhage. Additionally, prior publications have documented similar negative KB tests (no evidence of fetal-maternal blood transfer) despite the clinical diagnosis of abruption. This is due to the low sensitivity of the test as it has been reported to require 5 mL or more of fetal bleed into the maternal circulation for a positive result whereas only 0.01 to 0.05 mL of fetal-maternal bleed has been estimated to result in maternal sensitization [5]. The patient was informed of the clinical significance of this finding and the clinical implication for future pregnancies and the possible risk of erythroblastosis fetalis with a susceptible fetus. Ebner et al summarized the significance of this case report within their publication: “As a medical professional, the recommendation ‘don’t jump during pregnancy’ is undoubtedly the safest approach for mother and child” [1].
Beyond the rarity and novel nature of habitual skydiving while pregnant, this case underscores the need for increased access to contraceptive agents, especially for those persons with physical risk-taking behaviors. The ACOG has supported over-the-counter access to hormonal contraception without age restrictions [6]. While the Food and Drug Administration (FDA) is considering approving the United States’ first over-the-counter, progestin-only oral contraceptive pill [7], wider access to all forms of contraception, especially in the current post Roe V. Wade climate, would allow reproductive age women more precautions against unplanned pregnancies.
Learning points
Although the ACOG lists the activity as one to avoid in pregnancy, women may underestimate potential complications from the event and may continue to skydive while pregnant or may do so inadvertently if unaware of their pregnancy. Addressing potential obstetrical risks of extreme physical activities and/or sports should be done with all reproductive-age females prior to any incidental pregnancies, especially if reliable birth control is not in use. The offering of effective contraception in appropriate reproductive age women not currently seeking conception, as well as increased access to contraception, should be advocated. Ascertaining high-risk behavior (sexual or physical) in reproductive-age women and providing appropriate risk-reduction strategies should be encouraged by obstetricians-gynecologists during routine office visits.
Acknowledgments
We acknowledge Dr. Michael Spohn, Texas A&M Integrated Medicine Campus Dean, for his support of medical student clinical research.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Hector O. Chapa, MD, as treating physician for this patient, solicited and accepted verbal informed consent from the patient to use this case presentation as a case report publication.
Author Contributions
Primary author: Hector O. Chapa (40%). Carley Hagar: secondary author and formatting (20%); Armand Tadjali: proofreading and editing (20%); Elias Perli: editorial review of journal requirements, formatting (20%).
Data Availability
The authors declare that data supporting the findings of this study are available within the article. Additionally, the medical data are located within the treating hospital’s electronic medical record (Meditech); any other data desired supporting the findings of this study are available from the corresponding author upon reasonable request.
| References | ▴Top |
- Ebner F, Wockel A, Janni W, Paterson H. Parachuting and pregnancy: what do we know about pregnant skydivers and the risks they are taking? Clin J Sport Med. 2014;24(6):468-473.
doi pubmed - Skydiving Safety. US Parachute Association. http://www.uspa.org/facts-faqs/safety. Accessed April 11, 2017.
- ACOG Committee Opinion No. 650: physical activity and exercise during pregnancy and the postpartum period. Obstet Gynecol. 2015;126(6):e135-e142.
doi pubmed - Ptovin J, Potvin G. Parachute opening shock basics. Paper presented at: Parachute Industry Association Symposium, January 30, 2001; San Diego, MO. www.pcprg.com/s01out.htm. Accessed April 11, 2017.
- Krywko DM, Yarrarapu SNS, Shunkwiler SM. Kleihauer Betke Test. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2022. Accessed December 29, 2022. https://www.ncbi.nlm.nih.gov/books/NBK430876/.
- Over-the-counter access to hormonal contraception: ACOG Committee Opinion, Number 788. Obstet Gynecol. 2019;134(4):e96-e105.
doi pubmed - https://www.reuters.com/legal/us-fda-review-perrigos-birth-control-pill-otc-use-november-2022-09-12/.
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
