| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website http://www.jcgo.org |
Original Article
Volume 1, Number 1, February 2012, pages 10-14
Increased Cys-C Levels in Hyperemesis Gravidarum
Cemil Bilira, d, Suleyman Akarsub, Nermin Akdemirb, Feyzi Gokosmanogluc
aZonguldak Karaelmas University School of Medicine, Department of Internal Medicine, Turkey
bAnkara Kecioren Teaching and Research Hospital, Department of Gynecology and Obstetric, Turkey
cVan Caldıran State Hospital, Department of Internal Medicine, Turkey
dCorresponding author: Cemil Bilir, Sultan Orhan mh 1145 sk no:14 Gebze/Kocaeli, Turkey
Manuscript accepted for publication October 26, 2011
Short title: Cystatin C and Hyperemesis
doi: https://doi.org/10.4021/jcgo4e
| Abstract | ▴Top |
Background: Serum cys-C is superior to serum creatinine as an index of GFR also it can be used to predict acute renal failure before the rise in serum creatinine. We aimed to investigate cys-C levels in pregnant patients with hyperemesis gravidaum because of volume loss of this common problem.
Method: Thirty-seven patients with hyperemesis gravidarum and 33 healthy controls were included the study. Serum cys-C and the other laboratory parameters compared with controls.
Results: The hyperemesis gravidaum group had higher levels of BUN; AST and ALT. Groups did not differ in age, weight, gestational week, hemoglobin, glucose or creatinine levels. Serum cys-C levels were also higher in the hyperemesis gravidaum group (1.007 vs 0.63, P 0.002). Stepwise multiple regression analysis with the dependent variable “Cys-C”. The model had two independent predictors and an R2 of 63.7 %. Predictors for cys-C were the number of vomiting episodes and the duration of hospitalization.
Conclusion: There is a significant correlation between both the number of vomiting episodes and the length of the hospital stay with cys-C levels in HG. Cys-C levels could serve as a beneficial marker (cys-C > 1 mg/L as a cut-off value) in the context of hospitalization criteria for HG in the outpatient clinic.
Keywords: Hyperemesis gravidarum; Cystatin C; Hospitalization
| Introduction | ▴Top |
Hyperemesis gravidarum (HG) is observed in approximately 2% of pregnancies [1]. HG involves persistent vomiting with a weight loss > 5% of pre-pregnancy body weight and ketonuria unrelated to other causes [2]. Etiology and pathogenesis of HG are unknown. Due to the presence of severe nausea and associated vomiting, the duration of hospitalization is typically increased, incurring additional economic costs.
The glomerular filtration rate (GFR) cannot be measured directly in clinical practice and most of the methods that estimate the GFR have some limitations [3-5]. Serum cys-C (cys-C) is commonly accepted as a better method with which to estimate GFR. Two meta-analyses showed that serum cys-C is superior to serum creatinine as an index of GFR (R2 of 0.92 vs. 0.74, P < 0.001) (3 - 5). Cys-C can also be used to predict acute renal failure before the rise in serum creatinine. One study showed that serum cys-C was increased by at least 50% 1, 5 and 6 days earlier than serum creatinine [6].
There are few studies that have evaluated cys-C in pregnancy. Cataldi et al. found higher levels of cys-C in pregnant women at term compared to the controls [7, 8]. Cys-C levels were also studied in pre-eclamptic pregnant women. The maternal plasma level of cys-C was found to be a good marker for the onset and severity of pre-eclampsia. A biopsy study also demonstrated a positive correlation with renal structure. In late pregnancy, the serum level of cys-C has been closely correlated to third trimester changes in the GFR in both normal pregnancy and preeclampsia [9-12].
No study to date has examined cys-C levels in HG pregnant patients. We therefore aimed to investigate cys-C levels in HG pregnant patients.
| Methods | ▴Top |
Patients
Thirty-seven patients with hyperemesis gravidarum and 33 healthy controls were evaluated in this study. Ethical approval was obtained, and informed consent was obtained from each patient. The study was performed according to the Helsinki Declaration. The study cohort was selected from an obstetrical outpatient population of a research hospital in Ankara.
HG was defined as persistent vomiting accompanied by weight loss of at least 5% of the before-pregnancy body weight and/or ketonuria unrelated to other causes and requiring hospital admission for vomiting or dehydration. The control group had only mild nausea without vomiting or any other symptoms. We excluded patients with any of the following diseases: coronary heart disease, diabetes, hypertension or any chronic disease that required patients to take medication.
Fasting (8 hours) blood samples were taken in the morning of the first visit of outpatient clinic from each patient and were centrifuged for 5 min at 3000 × g and stored at -80 °C until the time of analysis. Blood glucose, serum creatinine, blood urea nitrogen, aspartate and alanine aminotransferases, sodium, potassium, clorur and calcium electrolytes were measured using an automatic analyzer (Konelab 60i, Thermo Scientific, Finland). Serum thyroid stimulating hormone and free thyroid hormones were analyzed by the UniCel DxI 800 Access Immunoassay System (Diasorin Liaison, USA). Complete blood counts were measured using a COULTER LH 500 hematology analyzer (Beckman Coulter, USA). Cys-C samples were taken before admission of patients to the hospital also it was first visit of patients. Cys-C concentrations were measured using direct ELISA (Abbott, aeoroset, Turkey) according to the manufacturer’s instructions. The serum normal limit of cys-C was 0.47 - 1.09 mg/L.
Ultrasound exams were performed by the same radiologist blinded to the clinical characteristics of the patients. Patients were admitted to the hospital and intravenously hydrated. This process was followed by the reintroduction of oral intake. Dehydrated patients were supplemented with the appropriate electrolytes, vitamins and metoclopramide (5 to 10 mg) as needed.
Statistical analysis
Normally distributed data were presented as the mean (SD) for baseline and descriptive statistics and median and interquartile ranges for non-normally distributed data. Data with a normal distribution were analyzed using an unpaired t-test. The Mann-Whitney U-test was used to analyze non-normally distributed data. Multiple stepwise linear regressions were used when the dependent and independent variables were continuous. All P values were calculated as two-tailed. P < 0.05 was considered statistically significant. SPSS 15.0 was used for statistical calculations (SPSS Inc., Chicago, IL, USA).
| Results | ▴Top |
Baseline clinical and laboratory characteristics of the patients and controls are presented in Table 1. Groups did not differ in age, weight, gestational week, hemoglobin, glucose or creatinine levels. No patients or controls had any other systemic disease or took any medication. None of the pregnant women had multiparity or molar pregnancy. Five patients in the HG group had dehydration and two of the patients had hypotension, The HG group had higher levels of BUN, AST and ALT; P values were 0.005, 0.01 and 0.04, respectively. The patients also had significantly lower levels of sodium and TSH; P values were 0.004 and 0.03, respectively. Serum cys-C levels were also higher in the HG group (Fig. 1). In the HG group, 13 of 37 patients (35%) had elevated cys-C levels. In the control group, only one of 33 patients (3%) had elevated cys-C levels (P value 0.0023). Further analysis of the data included stepwise multiple regression analysis with the dependent variable “Cys-C”. The model had two independent predictors, an R2 of 63.7 %, and a predicted R2 of 61.6%. Predictors for cys-C were the number of vomiting episodes and duration of hospitalization.
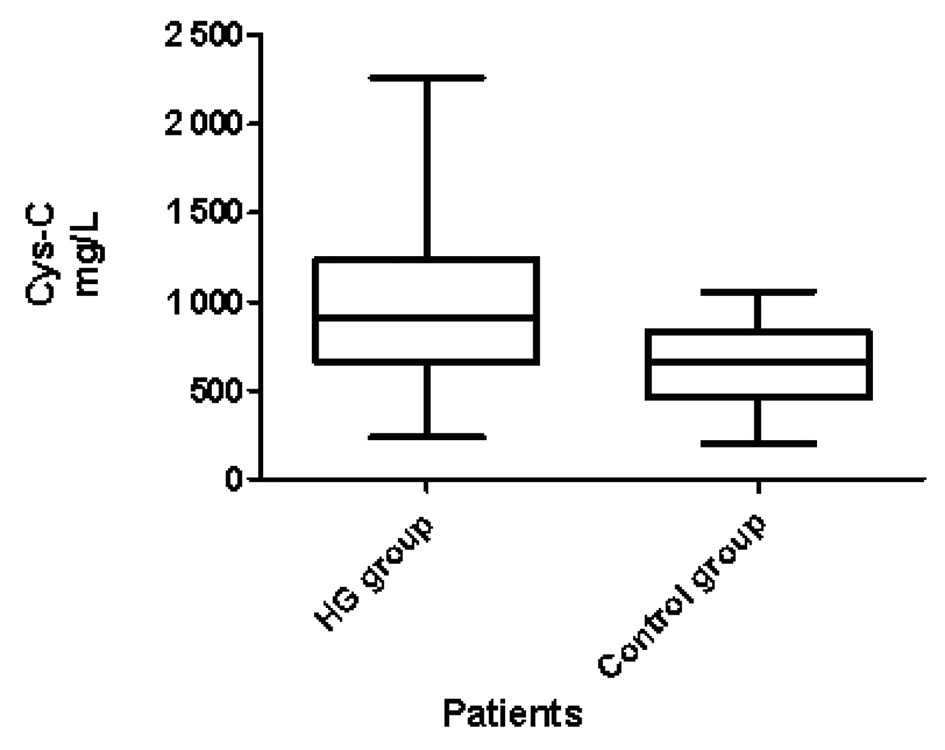 Click for large image | Figure 1. Cys-C levels in HG and controls. |
 Click to view | Table 1. Baseline Clinical and Laboratory Characteristics of 37 Patients With Hyperemesis Gravidarum and 33 Healthy Pregnant Controls |
| Discussion | ▴Top |
In this study, we found that cys-C levels were elevated in HG pregnant patients as compared to the controls. Furthermore, cys-C levels were a beneficial predictive marker of hospitalization time. The results of the present study suggest that cys-C levels (cut-off value > 1 mg/L) can be used as a criterion of hospital admission following the clinical assessment for HG patients. Therefore, Cys-C is a reliable marker in pregnant patients as well as in non-pregnant women. There are only few studies on cys-C levels in pregnant women. Strevens et al. found that cys-C is better than serum creatinine for estimating the GFR; other studies revealed that cys-C levels were higher in the third trimester. Later findings associated cys-C levels with inulin clearance and established that GFR was still markedly elevated in late pregnancy [8, 11-14]. There is only one published study that studied cys-C levels in the first trimester: values were between 0.45 - 0.6 mg/L in five pregnant patients [15]. We also found similar levels of cys-C in the control pregnant group (mean cys-C levels were 0.63 mg/L in 33 patients), as shown by Akbari et al.
The exact mechanism of elevated cys-C levels in preeclampsia is not known but may involve glomerular endotheliosis [16]. However, there is not any published data about glomerular endotheliosis or hyperemesis gravidarum. One of the other explanations for high cys-C levels may be fetal or placental weight. However, Strevens et al. did not find any correlation with these factors or cys-C in pre-eclamptic pregnant women [11].
It has been shown that hyperthyroidism and steroids may affect cys-C levels [17, 18]. Kotajima et al. found significantly higher serum concentrations of cys-C and TGF-β1 levels in patients with Graves' disease compared to controls [19]. One of the reasons for our findings could have been the elevated levels of cys-C in our study population, but there were no clinically hyperthyroid patients in our study population. Furthermore, multiple regression analysis did not show any statistically significant correlation between TSH, free T3 or free T4 and cys-C levels. Slayden et al. performed an animal study that showed that estradiol increased vaginal cys-C expression in fibroblasts [20]. Another study established the positive correlation with cys-C and serum leptin levels [21]. These hormonal changes may explain the elevated cys-C levels in HG.
BUN levels also significantly elevated in the HG group but there was no correlation with the csy-C levels, this may be a reason of oral hydration of patients prior to admission to the hospital.
Limitations: Small sample size and absence of leptin levels are study limitations.
Conclusion
There is a significant correlation between both the number of vomiting episodes and the length of the hospital stay with cys-C levels in HG. Cys-C levels could serve as a beneficial marker (cys-C > 1 mg/L as a cut-off value) in the context of hospitalization criteria following the clinical assessment for HG in the outpatient clinic.
Grant Support
We disclosure, we didn’t received support for this work from any organizations.
| References | ▴Top |
- Bailit JL. Hyperemesis gravidarium: Epidemiologic findings from a large cohort. Am J Obstet Gynecol. 2005;193(3 Pt 1):811-814.
pubmed doi - Goodwin TM. Hyperemesis gravidarum. Clin Obstet Gynecol. 1998;41(3):597-605.
pubmed doi - Madero M, Sarnak MJ, Stevens LA. Serum cystatin C as a marker of glomerular filtration rate. Curr Opin Nephrol Hypertens. 2006;15(6):610-616.
pubmed doi - Dharnidharka VR, Kwon C, Stevens G. Serum cystatin C is superior to serum creatinine as a marker of kidney function: a meta-analysis. Am J Kidney Dis. 2002;40(2):221-226.
pubmed doi - Laterza OF, Price CP, Scott MG. Cystatin C: an improved estimator of glomerular filtration rate? Clin Chem. 2002;48(5):699-707.
pubmed - Herget-Rosenthal S, Marggraf G, Husing J, Goring F, Pietruck F, Janssen O, Philipp T, et al. Early detection of acute renal failure by serum cystatin C. Kidney Int. 2004;66(3):1115-1122.
pubmed doi - Filler G, Bokenkamp A, Hofmann W, Le Bricon T, Martinez-Bru C, Grubb A. Cystatin C as a marker of GFR—history, indications, and future research. Clin Biochem. 2005;38(1):1-8.
pubmed doi - Cataldi L, Mussap M, Bertelli L, Ruzzante N, Fanos V, Plebani M. Cystatin C in healthy women at term pregnancy and in their infant newborns: relationship between maternal and neonatal serum levels and reference values. Am J Perinatol. 1999;16(6):287-295.
pubmed doi - Kristensen K, Larsson I, Hansson SR. Increased cystatin C expression in the pre-eclamptic placenta. Mol Hum Reprod. 2007;13(3):189-195.
pubmed doi - Strevens H, Wide-Swensson D, Grubb A. Serum cystatin C is a better marker for preeclampsia than serum creatinine or serum urate. Scand J Clin Lab Invest. 2001;61(7):575-580.
pubmed doi - Strevens H, Wide-Swensson D, Torffvit O, Grubb A. Serum cystatin C for assessment of glomerular filtration rate in pregnant and non-pregnant women. Indications of altered filtration process in pregnancy. Scand J Clin Lab Invest. 2002;62(2):141-147.
pubmed doi - Strevens H, Wide-Swensson D, Grubb A, Hansen A, Horn T, Ingemarsson I, Larsen S, et al. Serum cystatin C reflects glomerular endotheliosis in normal, hypertensive and pre-eclamptic pregnancies. BJOG. 2003;110(9):825-830.
pubmed doi - Davison JM, Hytten FE. Glomerular filtration during and after pregnancy. J Obstet Gynaecol Br Commonw. 1974;81(8):588-595.
pubmed doi - Krutzen E, Olofsson P, Back SE, Nilsson-Ehle P. Glomerular filtration rate in pregnancy: a study in normal subjects and in patients with hypertension, preeclampsia and diabetes. Scand J Clin Lab Invest. 1992;52(5):387-392.
pubmed doi - Akbari A, Lepage N, Keely E, Clark HD, Jaffey J, MacKinnon M, Filler G. Cystatin-C and beta trace protein as markers of renal function in pregnancy. BJOG. 2005;112(5):575-578.
pubmed doi - Lindheimer MD, Mahowald MB. Glomerular endotheliosis in normal pregnancy and pre-eclampsia. BJOG. 2004;111(2):191; author reply 193-195; discussion 195.
pubmed doi - Wiesli P, Schwegler B, Spinas GA, Schmid C. Serum cystatin C is sensitive to small changes in thyroid function. Clin Chim Acta. 2003;338(1-2):87-90.
pubmed doi - Risch L, Herklotz R, Blumberg A, Huber AR. Effects of glucocorticoid immunosuppression on serum cystatin C concentrations in renal transplant patients. Clin Chem. 2001;47(11):2055-2059.
pubmed - Kotajima N, Yanagawa Y, Aoki T, Tsunekawa K, Morimura T, Ogiwara T, Nara M, et al. Influence of thyroid hormones and transforming growth factor-beta1 on cystatin C concentrations. J Int Med Res. 2010;38(4):1365-1373.
pubmed - Slayden OD, Hettrich K, Carroll RS, Otto LN, Clark AL, Brenner RM. Estrogen enhances cystatin C expression in the macaque vagina. J Clin Endocrinol Metab. 2004;89(2):883-891.
pubmed doi - Retnakaran R, Connelly PW, Harris SB, Zinman B, Hanley AJ. Cystatin C is associated with cardiovascular risk factors and metabolic syndrome in Aboriginal youth. Pediatr Nephrol. 2007;22(7):1007-1013.
pubmed doi
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
