| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website http://www.jcgo.org |
Case Report
Volume 4, Number 1, March 2015, pages 179-183
Successful Surgical Removal of Symptomatic Intravenous Leiomyomatosis With Intracardiac Extension Completely Tamponating the Entire Right Atrium and Ventricle
Aline Tenzera, e, Jan Sebastian Wolterb, Stefan Gattenlohnerc, Peter Rothd, Ahmed Koshtyd, Hans-Rudolf Tinneberga
aDepartment of Gynecology and Obstetrics, University of Giessen and Marburg, Klinikstrasse 33, 35392 Giessen, Germany
bDepartment of Cardiology, Kerckhoff Heart and Thorax Centre Bad Nauheim, Benekestrasse 2-8, 61231 Bad Nauheim, Germany
cDepartment of Pathology, University of Giessen and Marburg, Klinikstrasse 33, 35392 Giessen, Germany
dDepartment Cardiovascular Surgery, University of Giessen and Marburg, Klinikstrasse 33, 35392 Giessen, Germany
eCorresponding Author: Aline Tenzer, Department of Gynecology and Obstetrics, University Hospital Giessen, Klinikstr. 33, 35392 Giessen, Germany
Manuscript accepted for publication October 17, 2014
Short title: Removal of Symptomatic Intravenous Leiomyomatosis
doi: http://dx.doi.org/10.14740/jcgo266w
| Abstract | ▴Top |
As a rare benign tumor, intravenous leiomyomatosis (IVL) can spread into the heart and lead to severe cardiac symptoms. A 50-year-old woman presented with progredient dyspnoea after hysterectomy for intrauterine leiomyoma 2 years ago. Diagnostic imaging revealed a tumor in the right atrium continuing from the right ovary passing within the right ovarian vein and the dilated inferior vena cava. The patient underwent a one-stage combined surgical operation with extracorporeal circulation in cooperation with gynecologists, cardiac surgeons and vascular surgeons. The tumor could be removed en bloc by access from the right atrium. The histological examination revealed IVL after hysterectomy.
Keywords: Leiomyomatosis; Dyspnoea; Hysterectomy; Cardiac tumor
| Introduction | ▴Top |
While leiomyoma is one of the most frequent tumors in females [1], intravenous leiomyomatosis (IVL) is rarely observed [2].
IVL is a rare benign intravascular tumor, and the tissue of origin is not absolutely clear [3].
Concerning the etiology and pathophysiology of this tumor, there exist two theories: some suggest tumor origin from smooth muscle cells of the vessel wall, and others discuss a subsequent invasion of venous channels with origin from uterine leiomyoma [4, 5].
Although histologically benign, IVL might be malignant in behavior [6]. It grows within the lumen of pelvic and systemic veins [7] and thereby reaches the right heart and rarely even the main pulmonary artery [8-10].
Depending on location and intravascular invasion, IVL can cause severe cardiorespiratory symptoms, mainly symptoms of right-sided heart congestion such as dyspnea, chest pain, syncope as well as edema [9, 11]. If not detected or if diagnosed too late, IVL has potentially life-threatening consequences [2, 11].
Surgical excision is the treatment of choice for IVL and complete removal of the tumor is necessary to prevent recurrence [9].
| Case Report | ▴Top |
A 50-year-old female, IG/IP, presented to her local cardiologist with progredient exercise-induced dyspnea and fatigue. The patient’s medical history was empty; her surgical history comprised a vaginal hysterectomy for intrauterine leiomyoma in 2011 and breast reduction surgery in 2002.
In echocardiography, a tumor within the right heart was detected and the patient was transferred to Kerckhoff Heart and Thorax Centre Bad Nauheim for further diagnostic investigation. Echocardiography and CT could confirm an intracardiac tumor of 8.75 × 4.34 cm extending the whole right atrium and ventricle with continuation of at least 12 cm into the vena cava inferior (Fig. 1, 2). The vena cava inferior was dilated to 28 mm. The diastolic function was slightly impaired (E/E’ med = 17), and the systolic function was normal.
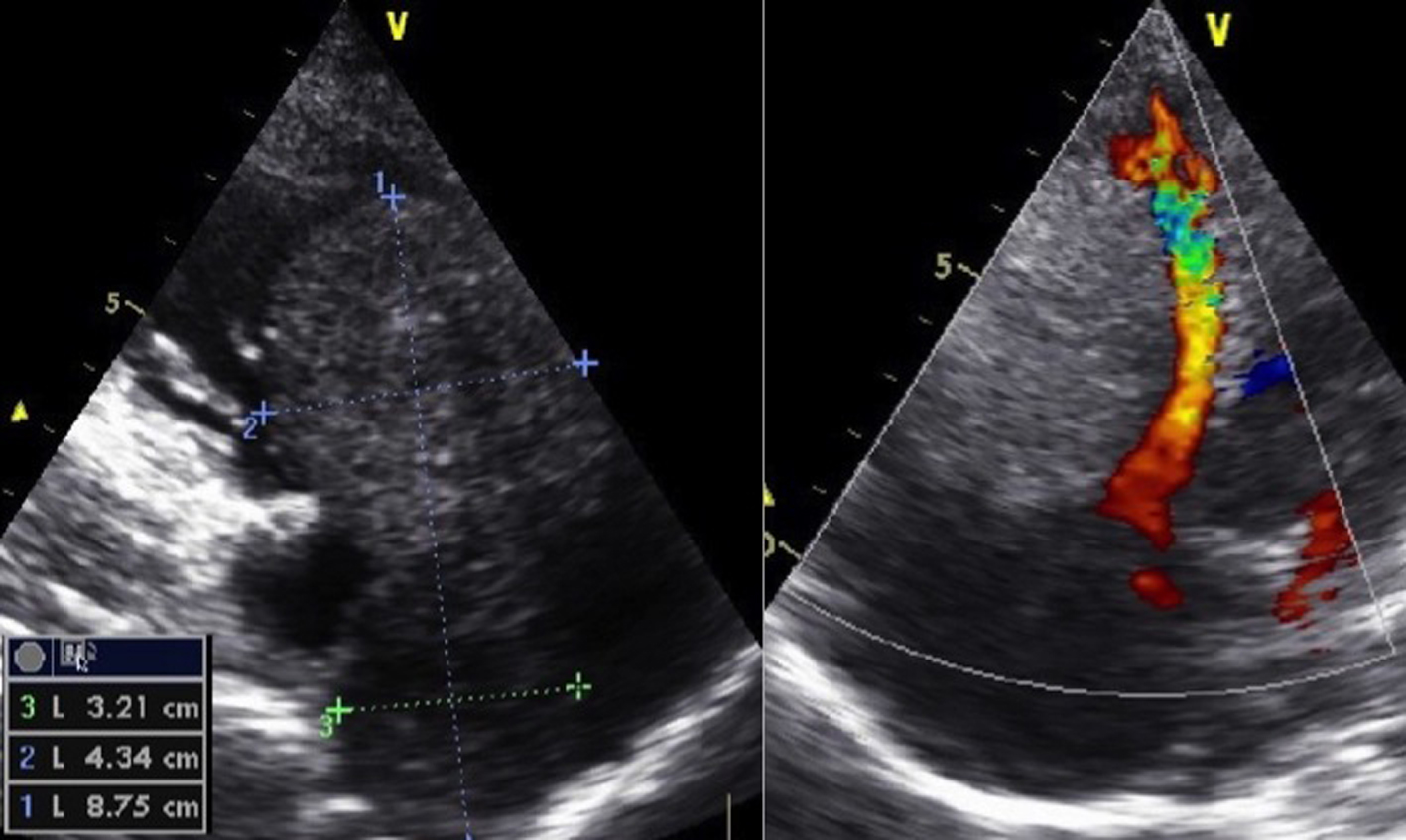 Click for large image | Figure 1. Modified five-chamber view of intracardiac tumor in the right ventricle. |
 Click for large image | Figure 2. CT scan of the intracardiac tumor in the right ventricle. |
For exclusion of pulmonary embolism, a CT scan was performed and a prophylactically anticoagulation with phenprocoumon commenced. The CT also revealed ascites and an enlarged right ovary of about 8 cm with a suspect mass disseminating into the dilated right ovarian vein and continuing in the vena cava to the right heart.
Because of these findings, a malignant neoplasm with origin from the right ovary was suspected and the patient was transferred to the Department of Gynecology and Obstetrics at the University Clinic of Giessen.
A performed ascetic tap revealed no malignant cells. The laboratory examinations were normal.
An explorative laparotomy and thoracotomy was discussed with the patient. The surgical setting with need of extracorporeal circulation was planned in cooperation with the vascular surgeons and cardiac surgeons. The patient gave her informed consent. In interval before surgery, the medication from phenprocoumon was shifted to fondaparinux.
The patient underwent a one-stage combined sternolaparotomy. First the median laparotomy was performed and the tumor within the right ovary was mobilized and dissected together with the mass at the beginning of the dilated ovarian vein (Fig. 3). The left adnexa were also removed. After that, the ovarian vein was dissected at half of its length and sent as frozen section.
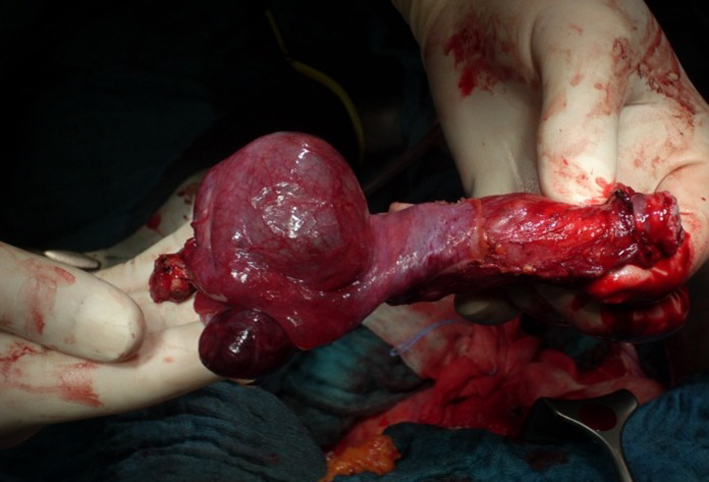 Click for large image | Figure 3. Intraoperative preparation. |
Further removal of the tumor mass in the remaining ovarian vein was performed by the vascular surgeon and finally handed over to the cardiac surgeon.
A median sternotomy was performed and the pericardial sac was opened. Cardiopulmonary bypass was instituted between the ascending aorta, the superior vena cava, and the right femoral vein. The right atrium was opened and the tumor of 3 - 4 cm with smooth surface and with continuation from vena cava inferior presented (Fig. 3). It was not adherent at any position in the heart. As next step the outlet of ovarian vein into vena cava inferior was dissected and the tumor was extracted en bloc by the access from the right atrium. Transesophageal echocardiography (TEE) was performed to confirm complete removal of the tumor.
After operation the patient was transferred to the surgical intensive care unit. The intraoperative frozen section revealed a benign tumor most likely IVL. These results were confirmed in final analysis.
The patient was discharged from hospital 12 days later. A therapeutic anticoagulation with phenprocoumon was recommended for the 12 following months.
The first follow-up examination after 3 months was completely normal without any evidence for recurrence.
| Discussion | ▴Top |
IVL was first described in 1896 by Birsch-Hirschfeld in an autopsy case [12]. The first case of IVL with intracardiac extension was described by Durck in 1907 [13].
In most cases, the extension of IVL is limited to the pelvic veins but can occasionally extend to IVC and the right heart [3]. But even extension of the IVL into pulmonary circulation has been described in literature [3, 8, 14] as well as association with multiple pulmonary metastases, despite the fact that IVL is a benign lesion [15].
IVL exclusively occurs in females, and the majority have undergone previous hysterectomy for intrauterine leiomyoma [16] with median time interval between hysterectomy and diagnosis of IVL of 4 years [17]. But even intervals of 20 years have been reported [18]. Lam et al reviewed 68 cases of intracardiac leiomyomatosis reported in the English literature between 1900 and 2003 and found that almost 56% of patients had prior hysterectomy [17]. They presumed that in these cases IVL in pelvic veins was undiagnosed in the early stage at the time of hysterectomy and for that reason could extend via the major vessels to the heart [17].
The here presented patient also underwent hysterectomy for intrauterine leiomyomatosis 2 years before diagnosis of IVL.
Concerning the etiology of IVL, two main theories exist: 1) IVL arises from the wall of the veins and 2) IVL is due to intravascular invasion of intrauterine leiomyoma [4, 5]. Norris and Parmley found in 14 reviewed cases evidence for both of these theories [4]. Finally, the exact etiology of IVL still remains unclear.
Patients with IVL involving the heart present with sometimes severe cardiac symptoms due to venous obstruction or decreased venous return to the heart [16]. In our case, the patient had ascites and an enlarged right ovary of about 8 cm. In combination with the ascites, a malignant disease was suspected. Postoperative histology revealed hemorrhagic benign ovarian cysts.
IVL is often misdiagnosed before histology is obtained after surgery [16] as it was the case in our patient where diagnosis of IVL was revealed also only after histopathological examination. Sudden death due to intracardiac extension has been reported in the literature, where IVL is only diagnosed postmortem [19].
Apart from primary cardiac tumors, thrombus from other intra-abdominal tumors as well as primary vascular tumors needs to be considered for differential diagnosis (Table 1) [9, 16, 20-25]. One of the most difficult differential diagnosis of IVL is leiomyosarcoma [16, 26]. In malignant leiomyosarcoma histology shows elevated mitosis rate compared to IVL [26].
 Click to view | Table 1. Differential Diagnosis of IVL |
In our patient the mitosis rate was low with 4 per 50 HPF.
Concerning treatment of IVL, surgery is the treatment of choice [11, 17]. Complete removal of the tumor is mandatory to avoid re-surgery [17]. The risk of recurrence amounts up to 30% in case of incomplete surgery [27]. Bilateral oophorectomy is recommended because IVL is estrogen-dependent [28]. In our patient, it was performed because of suspicion of malignancy.
Immunochemistry found estrogen and also progesterone receptor expression in tumor cells of IVL [29]. Kokawa et al found that IVL was related to overexpression of tissue estrogen receptor and high concentration of serum estradiol [30]. As IVL is estrogen-dependent, tamoxifen can inhibit tumor growth, so that it can be a treatment option for patients with incompletely resected tumor or postoperative residual tumor cells [24, 31].
With presence of intracardiac extension a multidisciplinary surgical approach is necessary which can be performed by a one-stage procedure through combined sternolaparotomy or two-stage procedure, if the tumor is too extensive or adherent to vascular or cardiac wall [2, 11, 17, 32]. In most cases described in literature, the extension of the tumor to the heart necessitates sternotomy or thoracotomy and frequently catheterization for cardiopulmonary bypass, whereas some reports of successful removal of IVL via laparotomy without need for entering the chest surgically exist [3, 16, 33]. Our patient had one-stage combined sternolaparotomy with cardiopulmonary bypass. But contrary to the findings in our patient, IVL reported by Matsuo et al without need for thoracotomy was of relatively small caliber without blockage of venous return to the heart and there was no apparent extension into the right atrium [33]. Furthermore, the IVL as benign tumor in this case was known preoperatively whereas the diagnosis in our patient was not clear at time of operation.
The intervention in our patient was without any complications; she was discharged 12 days after surgery with subjective well-being and the relief of not being affected by a malignant tumor.
In conclusion, IVL as rare benign tumor should be considered in women with cardiac symptoms and a right-sided intracardiac mass especially in combination with pelvic masses or with previous hysterectomies for leiomyoma. Total excision of the tumor is necessary to prevent recurrences and should be performed in a single or staged procedure if possible.
| References | ▴Top |
- Robboy SJ, Bentley RC, Butnor K, Anderson MC. Pathology and pathophysiology of uterine smooth-muscle tumors. Environ Health Perspect. 2000;108(Suppl 5):779-784.
doi pubmed - Clay TD, Dimitriou J, McNally OM, Russell PA, Newcomb AE, Wilson AM. Intravenous leiomyomatosis with intracardiac extension - a review of diagnosis and management with an illustrative case. Surg Oncol. 2013;22(3):e44-52.
doi pubmed - Derubertis BG, Clair D, Faries P, Kapur S, Park K, Kent KC. Resection of an intravenous leiomyoma with intracardiac extension with use of endovascular techniques. J Vasc Surg. 2004;40(3):554-558.
doi pubmed - Norris HJ, Parmley T. Mesenchymal tumors of the uterus. V. Intravenous leiomyomatosis. A clinical and pathologic study of 14 cases. Cancer. 1975;36(6):2164-2178.
doi - Borland DS, Wotring JW. Intravenous Leiomyomatosis of the Uterus and Broad Ligament. Report of a Case. Am J Clin Pathol. 1964;42:182-188.
pubmed - Diakomanolis E, Elsheikh A, Sotiropoulou M, Voulgaris Z, Vlachos G, Loutradis D, Michalas S. Intravenous leiomyomatosis. Arch Gynecol Obstet. 2003;267(4):256-257.
pubmed - Polizzi V, Pergolini A, Zampi G, Lo Presti M, Pino PG, Cartoni D, Sbaraglia F, et al. Intravenous leiomyomatosis extending to the heart: a multimodality imaging approach. Herz. 2014;39(6):720-721.
doi pubmed - Nishiwaki N, Konishi Y, Matsumoto M, Nishizawa J. [A case report of intravenous leiomyomatosis of the uterus with extension into the right pulmonary artery]. Nihon Kyobu Geka Gakkai Zasshi. 1989;37(12):2580-2585.
pubmed - Xu ZF, Yong F, Chen YY, Pan AZ. Uterine intravenous leiomyomatosis with cardiac extension: Imaging characteristics and literature review. World J Clin Oncol. 2013;4(1):25-28.
doi pubmed - Lee S, Kim DK, Narm KS, Cho SH. Pulmonary artery embolization of intravenous leiomyomatosis extending into the right atrium. Korean J Thorac Cardiovasc Surg. 2011;44(3):243-246.
doi pubmed - Low G, Rouget AC, Crawley C. Case 188: Intravenous leiomyomatosis with intracaval and intracardiac involvement. Radiology. 2012;265(3):971-975.
doi pubmed - Birsch-Hirchfeld FV. Lehrbuch der pathologischen Anatomie, 5th ed. Leipzig: FCW Vogel, 1896. p.26.
- Durck H. Ueber ein kontinuierlich durch die untere Hohlvene in das Herz vorwachsendes Fibromyom des Uterus. Munchen Med Wochenschr. 1907;54:1154-1155.
- Virzi G, Ragazzi S, Bussichella F, D'Agati P, Caputo S, Scaravilli F, Piazza D. Intravenous leiomyomatosis extending from the inferior caval vein to the pulmonary artery. J Thorac Cardiovasc Surg. 2007;133(3):831-832.
doi pubmed - Matsumoto K, Yamamoto T, Hisayoshi T, Asano G. Intravenous leiomyomatosis of the uterus with multiple pulmonary metastases associated with large bullae-like cyst formation. Pathol Int. 2001;51(5):396-401.
doi pubmed - Harris LM, Karakousis CP. Intravenous leiomyomatosis with cardiac extension: tumor thrombectomy through an abdominal approach. J Vasc Surg. 2000;31(5):1046-1051.
doi pubmed - Lam PM, Lo KW, Yu MY, Wong WS, Lau JY, Arifi AA, Cheung TH. Intravenous leiomyomatosis: two cases with different routes of tumor extension. J Vasc Surg. 2004;39(2):465-469.
doi pubmed - Payan MJ, Xerri L, Choux R, Gros N, Albrand JJ, Charpin C, Vaillant A, et al. [Giant leiomyoma of the inferior vena cava]. Ann Pathol. 1989;9(1):44-46.
pubmed - Roman DA, Mirchandani H. Intravenous leiomyoma with intracardiac extension causing sudden death. Arch Pathol Lab Med. 1987;111(12):1176-1178.
pubmed - Peng HJ, Zhao B, Yao QW, Qi HT, Xu ZD, Liu C. Intravenous leiomyomatosis: CT findings. Abdom Imaging. 2012;37(4):628-631.
doi pubmed - Bender LC, Mitsumori LM, Lloyd KA, Stambaugh LE, 3rd. AIRP best cases in radiologic-pathologic correlation: intravenous leiomyomatosis. Radiographics. 2011;31(4):1053-1058.
doi pubmed - Cleveland DC, Westaby S, Karp RB. Treatment of intra-atrial cardiac tumors. JAMA. 1983;249(20):2799-2802.
doi pubmed - Fasih N, Prasad Shanbhogue AK, Macdonald DB, Fraser-Hill MA, Papadatos D, Kielar AZ, Doherty GP, et al. Leiomyomas beyond the uterus: unusual locations, rare manifestations. Radiographics. 2008;28(7):1931-1948.
doi pubmed - Liu B, Liu C, Guan H, Li Y, Song X, Shen K, Miao Q. Intravenous leiomyomatosis with inferior vena cava and heart extension. J Vasc Surg. 2009;50(4):897-902.
doi pubmed - Huang J, Liu Q, Lu JP, Wang F, Wang L, Jin AG. Primary intraluminal leiomyosarcoma of the inferior vena cava: value of MRI with contrast-enhanced MR venography in diagnosis and treatment. Abdom Imaging. 2011;36(3):337-341.
doi pubmed - Kuenen BC, Slee PH, Seldenrijk CA, Wagenaar SS. Intravenous leiomyomatosis complicated by Budd-Chiari syndrome. Postgrad Med J. 1996;72(853):686-688.
doi pubmed - Ahmed M, Zangos S, Bechstein WO, Vogl TJ. Intravenous leiomyomatosis. Eur Radiol. 2004;14(7):1316-1317.
doi pubmed - Mitsuhashi A, Nagai Y, Sugita M, Nakajima N, Sekiya S. GnRH agonist for intravenous leiomyomatosis with cardiac extension. A case report. J Reprod Med. 1999;44(10):883-886.
pubmed - Kir G, Kir M, Gurbuz A, Karateke A, Aker F. Estrogen and progesterone expression of vessel walls with intravascular leiomyomatosis; discussion of histogenesis. Eur J Gynaecol Oncol. 2004;25(3):362-366.
pubmed - Kokawa K, Yamoto M, Yata C, Mabuchi Y, Umesaki N. Postmenopausal intravenous leiomyomatosis with high levels of estradiol and estrogen receptor. Obstet Gynecol. 2002;100(5 Pt 2):1124-1126.
doi - Du J, Zhao X, Guo D, Li H, Sun B. Intravenous leiomyomatosis of the uterus: a clinicopathologic study of 18 cases, with emphasis on early diagnosis and appropriate treatment strategies. Hum Pathol. 2011;42(9):1240-1246.
doi pubmed - Topcuoglu MS, Yaliniz H, Poyrazoglu H, Tokcan A, Demir SC, Bozkurt A, Zeren H. Intravenous leiomyomatosis extending into the right ventricle after subtotal hysterectomy. Ann Thorac Surg. 2004;78(1):330-332.
doi - Matsuo K, Fleischman F, Ghattas CS, Gabrielyan AS, Ballard CA, Roman LD, Morrow CP. Successful extraction of cardiac-extending intravenous leiomyomatosis through gonadal vein. Fertil Steril. 2012;98(5):1341-1345 e1341.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
