| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website http://www.jcgo.org |
Case Report
Volume 3, Number 3, September 2014, pages 117-120
A Case of Complete Urorectal Septum Malformation Sequence: Successful Vesicoamniotic Shunting for Obstructive Uropathy
Yoshiaki Masekia, Sayako Ikedaa, Atsuko Okazakia, Ken Miyazakia, Kana Kihiraa, Madoka Furuhashia, b
aDepartment of Obstetrics and Gynecology, Japanese Red Cross Nagoya Daiichi Hospital, Nagoya, Japan
bCorresponding Author: Madoka Furuhashi, Department of Obstetrics and Gynecology, Japanese Red Cross Nagoya Daiichi Hospital, 3-35 Michishita-cho, Nakamura-ku, Nagoya 453-8511, Japan
Manuscript accepted for publication August 29, 2014
Short title: Vesicoamniotic Shunting of URSM Sequence
doi: https://doi.org/10.14740/jcgo283w
| Abstract | ▴Top |
Complete urorectal septum malformation (URSM) sequence is a severe malformation affecting the urinary, genital and alimentary tracts. It is highly lethal due to severe renal dysfunction and pulmonary hypoplasia. Here we present a case of complete URSM sequence, where vesicoamniotic shunts were placed during midtrimester for obstructive uropathy. A 29-year-old woman was found to have a fetal abdominal cyst at 10+6 weeks of gestation. Obstructive uropathy was diagnosed and a vesicoamniotic shunt was placed at 14+3 and 20+0 weeks of gestation. Subsequent ultrasound findings were suggestive of URSM sequence. The infant was delivered by cesarean section at 34+6 weeks of gestation, and complete URSM sequence was diagnosed after birth. Obstetricians should be attentive to the possibility of complete URSM sequence when prominently dilated lower abdominal cyst is detected by ultrasonography. This case is indicative of the usefulness of vesicoamniotic shunting for obstructive uropathy of complete URSM sequence.
Keywords: Urorectal septum malformation sequence; Obstructive uropathy; Vesicoamniotic shunt; Double-basket catheter; Ultrasonography
| Introduction | ▴Top |
Urorectal septum malformation (URSM) sequence was first described by Escobar et al [1] in 1987. It is a rare malformation with an incidence of 1 in 50,000 - 250,000 neonates. Wheeler and Weaver [2] defined partial URSM as a single perineal or anal opening draining a common cloaca along with an absent (imperforate) anus, which is sometimes called persistent cloaca in females. In contrast, absence of both perineal and anal opening is called complete URSM sequence, which is highly lethal due to severe renal dysfunction and pulmonary hypoplasia [3].
Midtrimester oligohydramnios is a high risk for lethal pulmonary hypoplasia [4]. Fetal lower urinary tract obstruction, if untreated, carries a mortality of up to 45% mainly due to the severe oligohydramnios being associated with pulmonary hypoplasia [5]. Even in those who survive the neonatal period, up to one-third may develop end-stage chronic renal impairment, necessitating dialysis or transplantation [6]. Thus, antenatal intervention is required earlier in pregnancy to improve the fetal prognosis.
Here we present a case of complete URSM sequence, where vesicoamniotic shunts were placed during midtrimester for obstructive uropathy to reduce or avoid renal parenchymal damage and chronic oligohydramnios that can adversely affect pulmonary development.
| Case Report | ▴Top |
A 29-year-old woman, para 0, was referred to our hospital for a fetal abdominal cyst at 10+6 weeks of gestation. Transvaginal ultrasonography demonstrated that the crown-rump length of the fetus was 32.6 mm, with an abdominal cyst, 9.2 mm in diameter. At 14+0 weeks of gestation, the fetal abdominal cyst was increasing in size, reaching 39 mm in diameter and occupying the whole abdominal cavity (Fig. 1A). Amniotic volume was substantially decreased, but no other apparent anomalies were observed. We judged that the cyst was bladder-enlarged due to a severe urethral stenosis or obstruction. After informed consent was obtained, vesicoamniotic shunt placement was performed at 14+3 weeks of gestation under intravenous anesthesia. Karyotype analysis was not examined because the woman and her family did not desire it. First, amnioinfusion with 50 mL of saline was undertaken using a 23-gauge puncture needle to create an amniotic fluid pocket for the placement of the distal segment of the shunt catheter. Then, a 16-gauge puncture needle with a trocar (5 Fr, outer diameter 1.6 mm; Hakko Co., Nagano, Japan) was inserted through the maternal abdomen into the fetal bladder under ultrasonographic guidance. The inner needle was removed, and a silicon double-basket catheter was inserted with a pusher (4.5 Fr, outer diameter 1.5 mm, extended length 6.5 cm; Hakko Co.) into the trocar. After ensuring that the first half of the catheter was in the fetal bladder, the catheter was allowed to expand to its preformatted open shape. The other end of the catheter was expanded in the same way by removing the pusher under ultrasound control. Following the procedure, the amniotic cavity was filled with fetal urine and the fetal bladder was decompressed (Fig. 1B). At 20+0 weeks of gestation, an enlarged fetal bladder (43.8 × 24.6 mm) was observed by ultrasonography. Although the maximum vertical pocket was 27.9 mm, shunt trouble, such as obstruction or migration, was suspected. Thus, a double-basket catheter was placed again in the same manner listed above. At 21+5 weeks of gestation, ultrasonography demonstrated a dilated bowel (33.2 × 10.3 mm) with a hyperechoic area inside (Fig. 2A) and intraperitoneal calcifications with acoustic shadowing (Fig. 2B). Scan of the perineum showed ambiguous genitalia with a phallus-like image by ultrasonography at 27+0 weeks of gestation (Fig. 2C). At 30+0 weeks of gestation, a cystic mass (52.9 × 44.8 mm) beside the bladder and ascites were shown. At 31+0 weeks of gestation, a slightly distended pelvis of the left kidney was observed. At 33+0 weeks of gestation, ascites were increasing (Fig. 2D), although amniotic volume was normal. The infant was delivered by cesarean section at 34+6 weeks of gestation in consideration of the marked alteration in the volume of ascites. The birth weight was 3,290 g, and the Apgar scores were 1 and 5 at 1 and 5 min, respectively. Neither the external urethral orifice nor the anus was found with a phallus-like structure at the perineum (Fig. 3). After percutaneous cystostomy, the newborn was transferred to a specialized hospital for newborns 1 day after birth, where colostomy was undertaken the same day. Cystography demonstrated that rectum, vagina and bladder communicated each other. Definitely, complete URSM sequence and female sex were diagnosed by operative findings. Although one shunt catheter was easily removed at cesarean section, the other one was found in the abdominal cavity and removed during colostomy. Following anoplasty, she was in good condition with appropriate development and normal respiratory and renal function at 2 years of age, although a vesicocutaneous fistula was necessary for urination because a too short urethra did not enable urethroplasty. According to history taking, there is no URSM sequence in relatives.
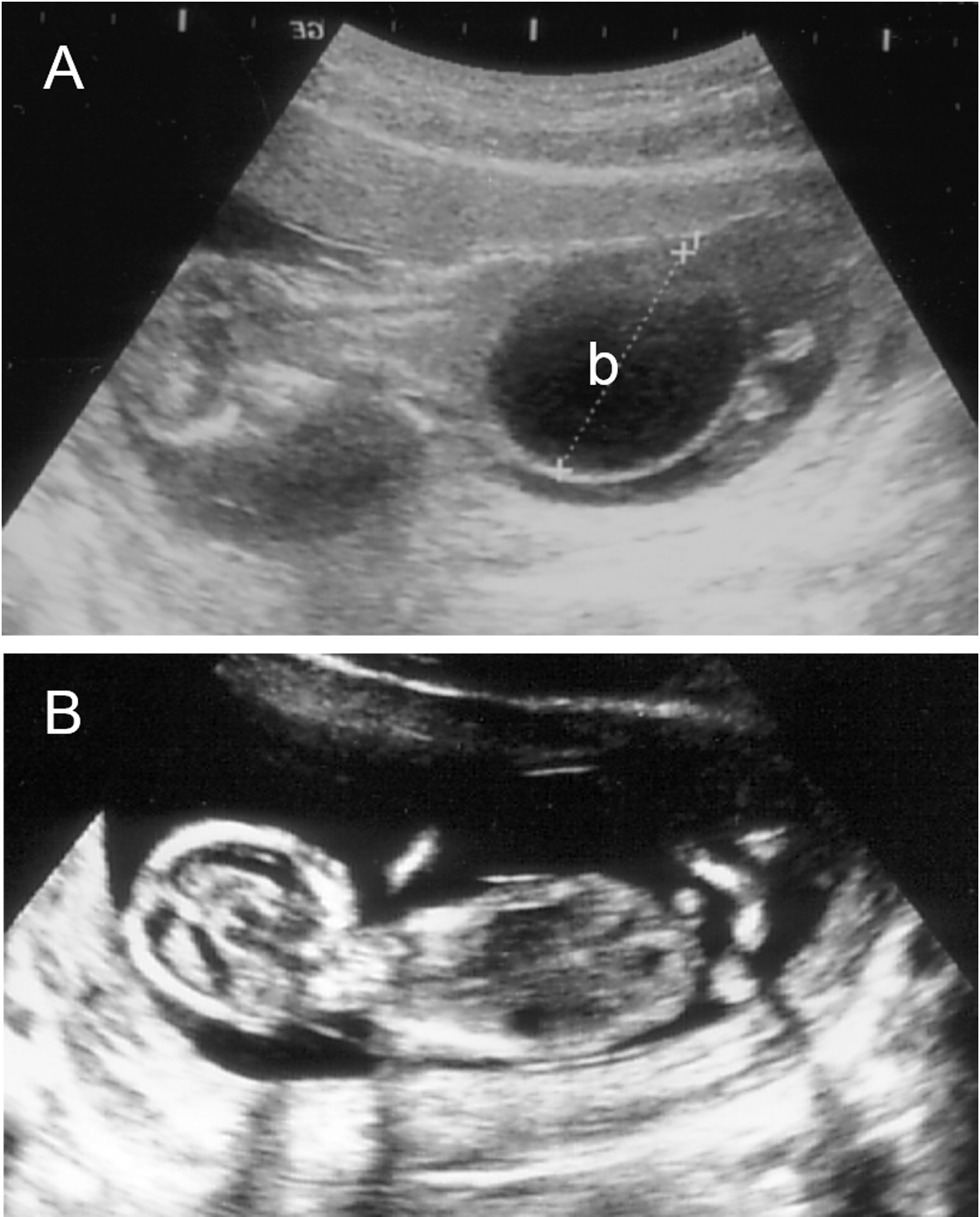 Click for large image | Figure 1. Longitudinal image of the fetus before (A) and after (B) the placement of a vesicoamniotic shunt. (A) 14+0 weeks of gestation; (B) 14+4 weeks of gestation. b: bladder. |
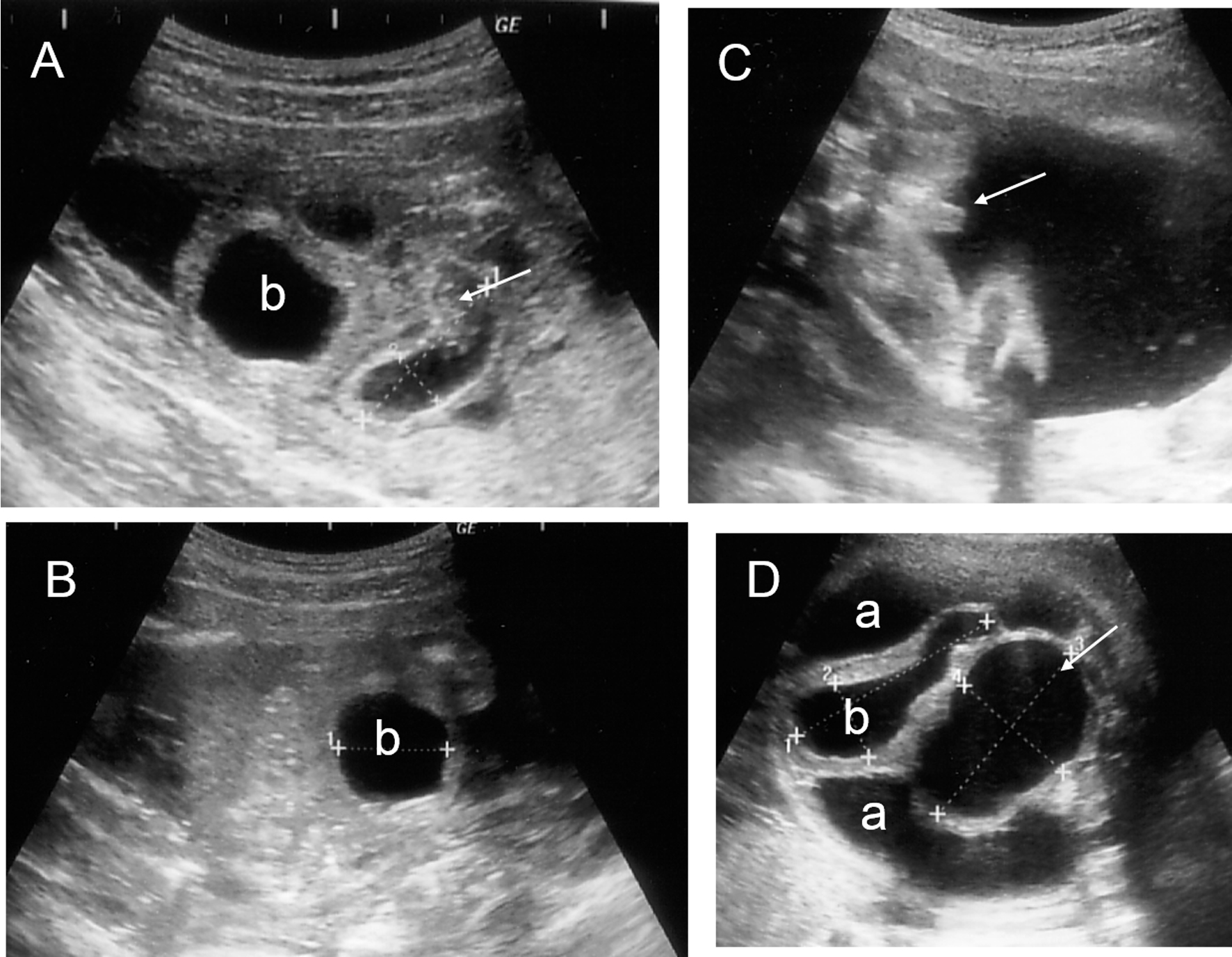 Click for large image | Figure 2. Fetal ultrasonography. Hyperechoic area (arrow) inside the dilated bowel (A) and intraperitoneal calcifications (B) were observed at 21+5 weeks of gestation. (C) A phallus-like image (arrow) was demonstrated at 27+0 weeks of gestation. (D) A cystic mass (arrow) beside the bladder and massive ascites were shown at 33+0 weeks of gestation. a: ascites; b: bladder. |
 Click for large image | Figure 3. Newborn baby just after birth. Abdomen was extraordinary dilated and a phallus-like structure was observed at the perineum. |
The study was approved by the Institutional Ethical Committee of Japanese Red Cross Nagoya Daiichi Hospital.
| Discussion | ▴Top |
Because of its rarity and the complex multisystem anatomic variation, URSM sequence is difficult to correctly diagnose prenatally. A cystic pelvic mass, urinary tract abnormalities, oligohydramnios and dilated bowel loops are the most common sonographic findings associated with URSM sequence [7]. Vijayaraghavan et al [8] reported that no visualization of the anus and intraluminal meconium calcification, which was caused by prolonged stasis of a mixture of fetal urine and meconium, were important signs in the prenatal sonographic diagnosis of URSM sequence. In the present case, the first finding was a huge bladder. With the progress of gestation, a cystic pelvic mass located posterior to the bladder, dilated bowel with hyperechoic area inside, intraperitoneal calcifications, and ascites, all of which suggested URSM sequence, were demonstrated by ultrasonography.
Complete URSM sequence is associated with a very poor prognosis. Hence, accurate prenatal diagnosis of this condition might allow termination of pregnancy with informed consent. When maintenance of pregnancy is desired, prevention of pulmonary hypoplasia and renal dysfunction is pivotal. According to Wheeler et al [9], three survivors out of 62 reported cases of URSM sequence had a patent urachus or bladder perforation that likely allowed for decompression of the urinary tract and contributed to increased amniotic fluid and fetal pulmonary development. In contrast to such a passive condition, Kanamori et al [10] first succeeded in vesicoamniotic shunting in complete URSM sequence at 27 weeks of gestation. The baby survived with preserved renal function, although moderate pulmonary hypoplasia was observed. Earlier vesicoamniotic shunting seems to guarantee a better prognosis of affected babies.
Harrison and Filly [11] reported that a predicted “good renal function”, shown as urine sodium and chloride concentrations, osmolarity, and urine output of less than 100 mEq/L, less than 90 mEq/L, less than 210 mOsm, and greater than 2 mL/h, respectively, is one of the selection criteria for vesicoamniotic shunt procedure. In the present case, vesicoamniotic shunting was performed without a functional evaluation of the potential for renal salvage based on the electrolyte and protein content of the urine. Over time, these original prognostic thresholds have been validated by many investigators. However, no consensus seems to have been reached as to the overall efficacy, and the use of urine electrolytes to determine renal prognosis requires additional refinements [5, 12]. Because the primary goal of fetal therapy for lower urinary tract obstruction is to prevent pulmonary hypoplasia, which is a main cause of neonatal death, the effects on renal or bladder function are secondary [12]. In the reported cases of poor renal function of newborns, the damage to the renal parenchyma might already have taken place at the time of vesicoamniotic shunting [13]. Therefore, an enlarged fetal bladder should be decompressed as early as possible, if fetal surgery is indicated. Early midtrimester, as in our case, may be an ideal time for vesicoamniotic shunting.
The fetal shunt procedure has been performed throughout the world, but the most common complication is shunt failure. Miyoshi et al [14] reported that the obstruction and displacement of the catheter were observed in 38% and 5% of thoracoamniotic shunting using a double-basket catheter for fetal chylothorax. Even in the present case, the enlarged fetal bladder was observed by ultrasonography at 20+0 weeks of gestation, suggesting obstruction or migration. Considering the risk, such as the spontaneous rupture of membranes and direct fetal death caused by shunting, the catheter is required to be thin, and hence, obstruction by amniotic fluid containing embryonum seems to be inevitable. Furthermore, catheters may migrate by fetal growth and movement. Actually, one catheter was displaced to the fetal abdominal cavity and was removed at postnatal colostomy. Motoi et al [15] reported persistent massive fetal ascites in persistent cloaca. Fetal ascites could be caused by urinary drainage through the fallopian tubes into the abdominal cavity; this cause of fetal ascites may be possible in the present case. Otherwise, the edge of the shunt-tube originally located in the amniotic cavity was displaced into the fetal abdominal cavity.
In conclusion, this case has shown that vesicoamniotic shunting for obstructive uropathy of complete URSM sequence is useful. Obstetricians should be attentive to the possibility of complete URSM sequence for timely placement of vesicoamniotic shunts when prominently dilated lower abdominal cyst is detected by ultrasonography.
Conflict of Interest
The authors do not have any conflicts of interest to declare.
| References | ▴Top |
- Escobar LF, Weaver DD, Bixler D, Hodes ME, Mitchell M. Urorectal septum malformation sequence. Report of six cases and embryological analysis. Am J Dis Child. 1987;141(9):1021-1024.
doi pubmed - Wheeler PG, Weaver DD. Partial urorectal septum malformation sequence: a report of 25 cases. Am J Med Genet. 2001;103(2):99-105.
doi pubmed - Williams DHt, Fitchev P, Policarpio-Nicolas ML, Wang E, Brannigan RE, Crawford SE. Urorectal septum malformation sequence. Urology. 2005;66(3):657.
- Winn HN, Chen M, Amon E, Leet TL, Shumway JB, Mostello D. Neonatal pulmonary hypoplasia and perinatal mortality in patients with midtrimester rupture of amniotic membranes—a critical analysis. Am J Obstet Gynecol. 2000;182(6):1638-1644.
doi pubmed - Freedman AL, Johnson MP, Gonzalez R. Fetal therapy for obstructive uropathy: past, present.future? Pediatr Nephrol. 2000;14(2):167-176.
doi pubmed - Parkhouse HF, Barratt TM, Dillon MJ, Duffy PG, Fay J, Ransley PG, Woodhouse CR, et al. Long-term outcome of boys with posterior urethral valves. Br J Urol. 1988;62(1):59-62.
doi pubmed - Jain D, Sharma MC, Kulkarni KK, Aggrawal S, Karak AK. Urorectal septum malformation sequence: a report of seven cases. Congenit Anom (Kyoto). 2008;48(4):174-179.
doi pubmed - Vijayaraghavan SB, Prema AS, Suganyadevi P. Sonographic depiction of the fetal anus and its utility in the diagnosis of anorectal malformations. J Ultrasound Med. 2011;30(1):37-45.
pubmed - Wheeler PG, Weaver DD, Obeime MO, Vance GH, Bull MJ, Escobar LF. Urorectal septum malformation sequence: report of thirteen additional cases and review of the literature. Am J Med Genet. 1997;73(4):456-462.
doi - Kanamori Y, Iwanaka T, Nakahara S, Kawashima H, Komura M, Sugiyama M, Kamei Y, et al. Survival in a neonate with complete urorectal septum malformation sequence after fetal vesico-amniotic shunting for a prominently dilated cloaca. Fetal Diagn Ther. 2008;24(4):458-461.
doi pubmed - Harrison MR, Filly RA. The fetus with obstructive uropathy: pathophysiology, natural history, selection, and treatment. In: Harrison MR, Golbus MS, Filly RA, eds. The Unborn Patient: Prenatal Diagnosis and Testament. Philadelphia: WB Saunders, 1991:328-393.
pubmed - Morris RK, Khan KS, Kilby MD. Vesicoamniotic shunting for fetal lower urinary tract obstruction: an overview. Arch Dis Child Fetal Neonatal Ed. 2007;92(3):F166-168.
doi pubmed - Morris RK, Malin GL, Quinlan-Jones E, Middleton LJ, Hemming K, Burke D, Daniels JP, et al. Percutaneous vesicoamniotic shunting versus conservative management for fetal lower urinary tract obstruction (PLUTO): a randomised trial. Lancet. 2013;382(9903):1496-1506.
doi - Miyoshi T, Katsuragi S, Ikeda T, Horiuchi C, Kawasaki K, Kamiya CA, Sasaki Y, et al. Retrospective review of thoracoamniotic shunting using a double-basket catheter for fetal chylothorax. Fetal Diagn Ther. 2013;34(1):19-25.
doi pubmed - Motoi M, Satoshi I, Takatsugu M, Masato K, Yuko M, Takuya T, Yuka F, et al. Persistent cloaca presenting with persistent massive fetal ascites resulting from severely compromised urinary function. Fetal Diagn Ther. 2009;25(2):183-185.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
